J Adv Periodontol Implant Dent. 2025;17(3):126-131.
doi: 10.34172/japid.025.3398
Research Article
Root coverage in Miller’s Class I and II gingival recession using acellular dermal matrix and subepithelial connective tissue graft: A systematic review
Aaesha I.A Khan Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Visualization, Writing – original draft, Writing – review & editing, , * 
Sujeet V. Khiste Conceptualization, Investigation, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, 
Vineet Kini Visualization,
Author information:
Department of Periodontics, Mahatma Gandhi Mission’s Dental College and Hospital, Navi Mumbai, Maharashtra University of Health and Science, Nashik, India
Abstract
Background.
Subepithelial connective tissue graft (SCTG) is considered the gold standard in the treatment of gingival recession. Donor site morbidity has led to the introduction of non-autogenous grafts such as acellular dermal matrix (ADM). This systematic review compared SCTG with ADM to treat root coverage in Miller’s Class I and Class II gingival recession.
Methods.
Articles in PubMed (11), Scopus (1), EBSCO (2), and Google Scholar (1) were incorporated in this study. The studies included randomized controlled trials from 1st January 2011 to 31st December 2022. Studies that compared root coverage and reduction in recession depth using SCTG and ADM grafts were included in the review. Fourteen randomized control trials (RCTs) were included in this systematic review following the PRISMA guidelines. The risk bias assessment was assessed using the ROBINS-2 tool.
Results.
Of the 14 included studies, 11 articles concluded that ADM is as effective as SCTG for treating root coverage in Class I and Class II gingival recession. However, 3 studies showed a statistically significant difference between SCTG and ADM results, indicating better root coverage achieved with SCTG than with ADM.
Conclusion.
ADMs may be an alternative treatment in cases where multiple areas of recession where SCTGs harvested from the palate area would be insufficient.
Keywords: Acellular dermal graft tissue, Allografts, Connective tissue, Gingival recession
Copyright and License Information
© 2025 The Author(s).
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Funding Statement
None.
Introduction
Displacement of the gingival margin apical to the cementoenamel junction (CEJ), leading to root surface exposure, is known as gingival recession.1 Various etiologic factors can result in gingival recession, such as tooth brushing trauma, restorations invading the biological width, improper brushing technique, plaque-induced inflammatory lesions, and surgical periodontal interventions. Gingival recession can lead to root hypersensitivity, root caries, and unpleasant esthetics, particularly in the anterior regions of the jaws.2 Subepithelial connective tissue graft (SCTG) is considered the gold standard in the treatment of gingival recessions for root coverage. It provides long-term stability of complete root coverage (CRC) in Miller’s Class I and Class II gingival recession. However, the main disadvantage of this technique is the need for a second surgical area, limited amount of graft, low patient tolerance, and high complication rates at the donor site.3
To overcome the limitations, new biomaterials, such as ADM, have been introduced as an alternative to SCTGs.4 ADM is an allograft tissue devoid of epidermal and dermal cells. It is chemically processed to remove the cellular components while preserving the remaining bioactive dermal matrix. This matrix consists of collagens, elastin, blood vessel channels, and bioactive proteins that induce revascularization, cell repopulation, and tissue remodeling. The collagen fibrillar network allows ADM to maintain its structural integrity, thereby giving it characteristics of a feasible soft tissue graft material.5
Various ADM materials are available on the market, such as Alloderm (LifeCell.Biohorizon INC), Puros dermis allograft, Perioderm, Oracell, Surederm, and Mucoderm, which can be effectively used to treat gingival recession and achieve root coverage.5
Al Hamdam6 assessed the long-term predictability of ADM in root coverage procedure with a follow-up of three years. The study showed that ADM combined with a coronally advanced flap could improve the width of keratinized tissue and provide root coverage in teeth with gingival recession.
Considering the various advantages of ADM, this systematic review compared root coverage in Miller’s Class I and II gingival recession using ADM and SCTG.
Methods
This systematic review was registered under PROSPERO (CRD42022362523) and conformed to PRISMA guidelines.7 The research question was based on patient/population, intervention, comparison, and outcomes (PICO). The research question of this systematic review was whether ADM (I) is as effective as connective tissue graft (C) in root coverage (O) of Miller’s Class I and Class II gingival recession (P).
The systematic review was performed for articles published in English in Scopus, PubMed, EBSCO, and Cochrane from 1st January 2011 to 31st December 2022. The terms were combined using suitable Boolean operators (AND, OR, NOT). The keywords used were acellular dermal graft tissue, allografts, autografts, connective tissue, gingival recession, and systematic review. The search strategy used was: “gingival recession” [MeSH terms] OR (“gingival” AND “recession” OR “gingival recession” AND (“acellular dermis” [MeSH Terms] OR (“acellular” AND “dermis” OR “acellular dermis” OR (“acellular” AND “dermal” AND “matrix” [all fields]) OR “acellular dermal matrix” AND (clinical trial) OR randomized controlled trial OR systematic review.
The inclusion criteria were randomized controlled trials comparing root coverage using ADM and subepithelial connective grafts to treat Miller’s Class I and Class II gingival recession. In vitro studies, animal models, case reports, reviews, abstracts, and unpublished articles were excluded.
According to the inclusion and exclusion criteria, one reviewer investigated the titles and abstracts of the studies, based on which two experts screened extracted articles from the database. Disagreements were resolved by discussion. The final step included all full-text articles for the study. The main outcome was to assess whether the ADM was better in improving root coverage in Class I and Class II gingival recession compared to connective tissue grafts.
Microsoft Word was used for organizing data extraction, which included the name of the author, year, study design, study duration, participants, parameters, surgical method, postoperative instructions, results, and conclusion. Two entries were used for blinding: (1) operators and (2) outcome assessors. Assessment risk of bias using ROBINS-2 for randomized studies and used as per Revised Cochrane risk-of-bias tool RevMan 5.4.1 for systematic review.
Two review authors independently undertook the risk of bias assessment. Any disagreements were resolved by discussion. The outcome of the trial was noted when the operator assessed it. The response options were Yes/Probably yes/Probably no/No/No information. There was good reliability between the two reviewers with a high kappa coefficient (k > 0.89).
The two-part tool addressed five specific domains (namely, randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result). The possible risk-of-bias judgments were assessed as low risk of bias, some concerns, and high risk of bias. Risk of bias were presented as summary review of authors’ judgments about risk of bias item for each study and overall percentages across all included studies.
Results
The systematic search resulted in 94 articles. After screening and removing the duplicates, the remaining 31 articles were included. A comprehensive assessment was conducted by the review team for the title of the articles and abstracts and after excluding the unrelated articles from the research objectives. Eventually, 15 articles were obtained after screening, out of which one was excluded due to the unavailability of the full text. Therefore, 14 articles were included, which is depicted in the form of a PRISMA screening flowchart (Figure 1). Based on the revised Cochrane risk-of-bias tool for randomized trials (RoB2) scoring system. Each included study demonstrated a low risk of bias (Figure 2). Overall the articles showed low risks of bias (Figure 3). Data obtained from the articles have been included in Table S1 (see Supplementary file 1).8-21 The study included a population with more than one gingival recession site. Included articles were randomized clinical trials.

Figure 1.
PRISMA flowchart
.
PRISMA flowchart
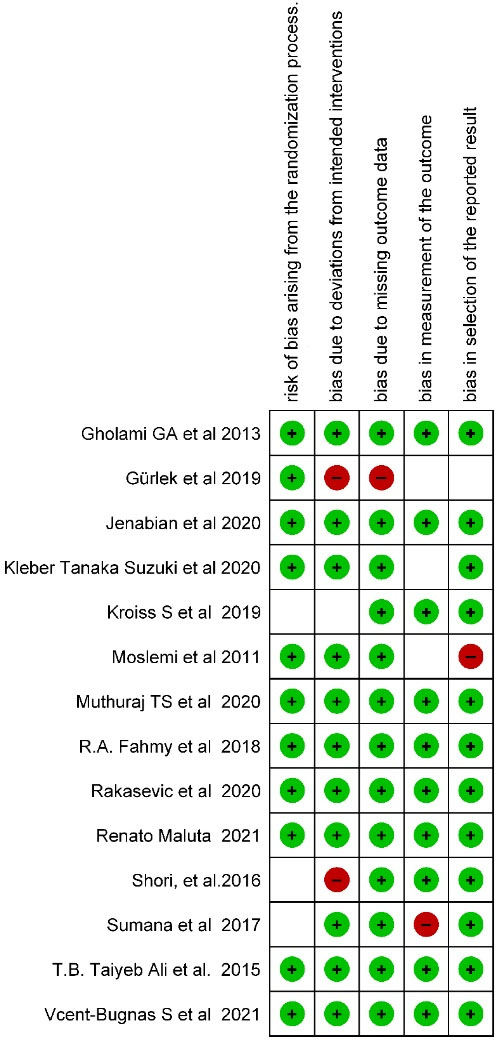
Figure 2.
Risk of bias summary: Review authors’ judgments about each risk of /bias item for each included study
.
Risk of bias summary: Review authors’ judgments about each risk of /bias item for each included study
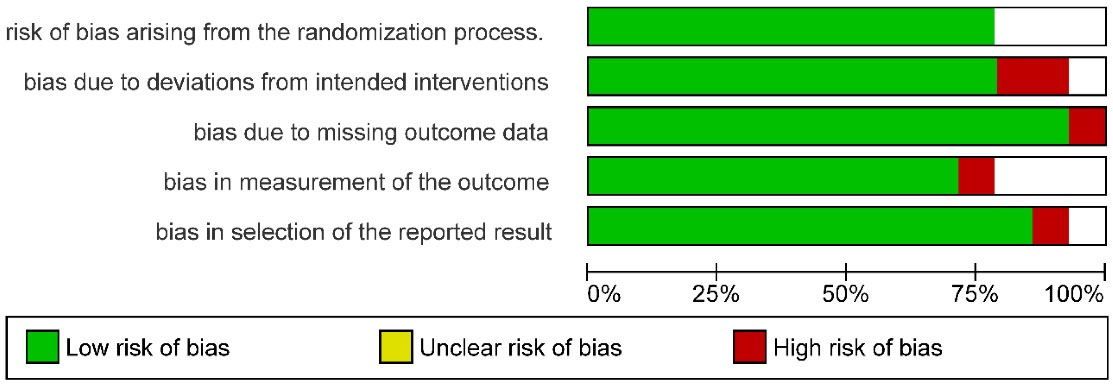
Figure 3.
Review authors’ judgments about each risk of bias item presented as percentage across all included studies
.
Review authors’ judgments about each risk of bias item presented as percentage across all included studies
Based on the data extracted from 14 studies, 11 articles concluded that ADM is as effective as SCTG for treating root coverage in Class I and Class II gingival recession. Statistically significant results were obtained in three studies, which favored SCTG over ADM for root coverage in Miller’s Class I and Class II gingival recession.10,17,21
Discussion
The purpose of the present systematic review was to compare root coverage in SCTG versus ADM in treating Miller’s Class I and Class II gingival recession. According to Chambrone et al,22 the root coverage produced by ADM was similar to those achieved by SCTG. Maluta et al17 conducted a comparative assessment between SCTG and ADM for root coverage. A statistically significant difference (P = 0.045) was seen at 6 months between SCTG and ADM, with better root coverage results observed in the SCTG group.17 In SCTG, preexisting blood vessels anastomose with those in the gingival connective tissue. ADM, being avascular, acts as a scaffold for cells from the surrounding tissues. The collagen fibers in the ADM membrane facilitate root coverage by stimulating platelet attachment, enhancing fibrin linkage, and having a chemotactic effect on nearby fibroblasts.23 The crosslinking of the ADM helps increase the tensile strength, stiffens the matrix and bulk of the graft, and reduces the porosity of the matrix. As healing proceeds, ADM is fully integrated into the host tissues. It completely depends on the recipient bed, which is eventually degraded and replaced by the host cell.24 Because of its elastic matrices and undamaged collagen fibrils, ADM can be used as a substitute for CTG in root coverage procedures. However, the disadvantages of using ADM include lack of vascularity, longer healing time, cost of the material, and postoperative management.24,25 Therefore, better root coverage results were in favor of SCTG than in the test group. Inductive properties of ADM graft are determined by the percentage of colonization of non-vital graft and host cells inducing keratinization. Connective tissue grafts are entirely made up of host cells and, hence, can induce epithelium keratinization.25
Owens et al26 reported increased resident fibroblasts and blood vessels gradually within the first few weeks and reduced inflammatory infiltrate. The graft material showed degradation of the collagen matrix at the fourth week. By six weeks there was formation of basement membrane with complete re-epithelialization of gingiva. Traces of ADM were also seen after 10 weeks.27,28 The present systematic review is consistent with a study by Wei et al.29 The study reported that an increase in the width of attached gingiva was observed with SCTG than with ADM graft, which could be attributed to the considerable shrinkage of ADM during the healing phase. SCTG harvested from the palate resulted in more postoperative pain, discomfort and ulceration of the flap because of the more extensive procedure. Hence, ADM can be used as an alternative to avoid multiple tissue harvesting, morbidity, and patient discomfort.30,31
In the present systematic review, both SCTG and ADM were equally effective in reducing the gingival recession depth and accomplishing root coverage. Moslemi et al14 evaluated root coverage using SCTG and ADM with a follow-up of 5 years. The study reported that mean root coverage was improved using both grafts at 6 months but decreased significantly over 5 years. The relapse of SCTG and ADM was attributed to the improper toothbrushing technique of the participants.14
Quality of the evidence
Randomized control trial (RCT) was assessed as low risk of bias. A more patient-centered outcome can be evaluated using a visual analog scale (VAS), a tool to assess the levels of discomfort and pain after different periodontal treatment modalities. This resource can help evaluate various esthetic and functional outcomes of an individual. A recent study using a VAS showed that pain and discomfort were more significant in the control group than in the test group. Postoperative bleeding, as well as soft tissue necrosis, was observed on the donor and recipient sites of the control group.11,14 Some studies demonstrated no signs of allergy, infection, or other complications were seen, indicating that ADM was well tolerated and accepted by the participants.15,16
According to Muthuraj et al,13 ADM showed better color matching as it provides a scaffold for the ingrowth of native cells from the recipient bed, giving a better esthetic result and inhibits the effect of the underlying connective tissue which influences epithelial cells by secretion of keratinocyte growth factor, reducing melanin pigmentation.
Some studies applied root modification agents (e.g., tetracycline solution, EDTA, and citric acid) in recession defects. Nevertheless, these RCTs suggested no significant clinical benefit of root conditioning in conjunction with root-coverage procedures.8,9,19
Overall, the results of this systematic review demonstrated a statistically significant reduction in the extent of GR and an associated gain in the clinical attachment level with or without improvements in the width of keratinized tissue in both control (SCTG) and test (ADM) groups. However, ADM has successfully emerged as an alternative for correcting multiple Class I and Class II gingival recession defects for functional and esthetic purposes.
Further RCTs are required to evaluate primarily in terms of esthetics, relapse, and secondary outcomes between different procedures. The inclusion of the recession defect type should have been balanced, and the difference in the treatment response of Class I and Class II recession sites should be considered. Limited data is available on the long-term follow-up of the patients treated for gingival recession. Meta-analyses could have given a definitive conclusion regarding the superiority of one graft over the other.
Conclusion
-
Both SCTG and ADM for treating Miller’s Class I and Class II gingival recession can achieve better root coverage and gain in the width of keratinized tissue.
-
ADM may be an alternative treatment in cases where multiple areas of recession are seen, where SCTGs harvested from the palate area would be insufficient.
-
Most cases produced significant gains in the clinical attachment level and width of keratinized tissue with differences in the percentages of CRC and mean root coverage.
-
SCTG might be considered a gold standard for treating recession-type defects; however, the incidence of discomfort and pain was directly related to donor sites of SCTG.
Within this study’s limitations, SCTG and ADM are equally effective for root coverage in Class I and Class II gingival recession. However, it is the clinician’s decision depending upon the clinical skills, patients’ willingness to undergo surgical procedures involving a donor site, and the cost required for the surgery.
Competing Interests
No competing interests.
Consent for Publication
Not applicable.
Data Availability Statement
The data are available upon request from the corresponding author.
Ethical Approval
Not applicable.
Supplementary Files
Supplementary file 1 contains Table S1.
(pdf)
References
- Mostafa D, Fatima N. Gingival recession and root coverage up to date, a literature review. Dent Rev 2022; 2(1):100008. doi: 10.1016/j.dentre.2021.100008 [Crossref] [ Google Scholar]
- Imber JC, Kasaj A. Treatment of gingival recession: when and how?. Int Dent J 2021; 71(3):178-87. doi: 10.1111/idj.12617 [Crossref] [ Google Scholar]
- Pini-Prato G. The Miller classification of gingival recession: limits and drawbacks. J Clin Periodontol 2011; 38(3):243-5. doi: 10.1111/j.1600-051X.2010.01655.x [Crossref] [ Google Scholar]
- Petrie K, Cox CT, Becker BC, MacKay BJ. Clinical applications of acellular dermal matrices: a review. Scars Burn Heal 2022; 8:20595131211038313. doi: 10.1177/20595131211038313 [Crossref] [ Google Scholar]
- Fosnot J, Kovach SJ 3rd, Serletti JM. Acellular dermal matrix: general principles for the plastic surgeon. Aesthet Surg J 2011; 31(7 Suppl):5S-12S. doi: 10.1177/1090820x11417576 [Crossref] [ Google Scholar]
- Al-Hamdan K. Long-term predictability of allogenic dermal matrix for root coverage: three years observation period on 15 consecutive cases. Saudi Dent J 2021; 33(2):99-104. doi: 10.1016/j.sdentj.2020.01.001 [Crossref] [ Google Scholar]
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009; 339:b2700. doi: 10.1136/bmj.b2700 [Crossref] [ Google Scholar]
- Gholami GA, Saberi A, Kadkhodazadeh M, Amid R, Karami D. Comparison of the clinical outcomes of connective tissue and acellular dermal matrix in combination with double papillary flap for root coverage: A 6-month trial. Dent Res J (Isfahan) 2013; 10(4):506-13. [ Google Scholar]
- Gürlek Ö, Gümüş P, Nizam N, Buduneli N. Coronally advanced flap with connective tissue graft or xenogeneic acellular dermal matrix in the treatment of multiple gingival recessions: a split-mouth randomized clinical trial. J Esthet Restor Dent 2020; 32(4):380-8. doi: 10.1111/jerd.12547 [Crossref] [ Google Scholar]
- Jenabian N, Yazdanpanahbahabadi M, Haghpanah Aski P, Bijani A. Comparison of acellular dermal matrix allograft (ADMA) and a subepithelial connective tissue graft (SCTG) for the treatment of gingival recession. J Adv Periodontol Implant Dent 2020; 12(1):11-7. doi: 10.34172/japid.2020.004 [Crossref] [ Google Scholar]
- Suzuki KT, de Jesus Hernandez Martinez C, Suemi MI, Palioto DB, Messora MR, de Souza SL. Root coverage using coronally advanced flap with porcine-derived acellular dermal matrix or subepithelial connective tissue graft: a randomized controlled clinical trial. Clin Oral Investig 2020; 24(11):4077-87. doi: 10.1007/s00784-020-03280-x [Crossref] [ Google Scholar]
- Kroiss S, Rathe F, Sader R, Weigl P, Schlee M. Acellular dermal matrix allograft versus autogenous connective tissue grafts for thickening soft tissue and covering multiple gingival recessions: a 5-year preference clinical study. Quintessence Int 2019; 50(4):278-85. doi: 10.3290/j.qi.a42160 [Crossref] [ Google Scholar]
- Muthuraj TS, Bagchi S, Bandyopadhyay P, Mallick S, Ghosh P, Renganath MJ. A randomized split mouth clinical study to compare the clinical outcomes of subepithelial connective graft and acellular dermal matrix in Miller’s class I recession coverage therapy. J Indian Soc Periodontol 2020; 24(4):342-7. doi: 10.4103/jisp.jisp_609_19 [Crossref] [ Google Scholar]
- Moslemi N, Mousavi Jazi M, Haghighati F, Morovati SP, Jamali R. Acellular dermal matrix allograft versus subepithelial connective tissue graft in treatment of gingival recessions: a 5-year randomized clinical study. J Clin Periodontol 2011; 38(12):1122-9. doi: 10.1111/j.1600-051X.2011.01789.x [Crossref] [ Google Scholar]
- Fahmy RA, Taalab MR. Modified tunnel technique for management of gingival recession in esthetic zone using acellular dermal matrix versus connective tissue graft. Futur Dent J 2019; 5(2):1-5. doi: 10.1016/j.fdj.2018.12.001 [Crossref] [ Google Scholar]
- Rakasevic DL, Milinkovic IZ, Jankovic SM, Soldatovic IA, Aleksic ZM, Nikolic-Jakoba NS. The use of collagen porcine dermal matrix and connective tissue graft with modified coronally advanced tunnel technique in the treatment of multiple adjacent type I gingival recessions: a randomized, controlled clinical trial. J Esthet Restor Dent 2020; 32(7):681-90. doi: 10.1111/jerd.12624 [Crossref] [ Google Scholar]
- Maluta R, Monteiro MF, Peruzzo DC, Joly JC. Root coverage of multiple gingival recessions treated with coronally advanced flap associated with xenogeneic acellular dermal matrix or connective tissue graft: a 6-month split-mouth controlled and randomized clinical trial. Clin Oral Investig 2021; 25(10):5765-73. doi: 10.1007/s00784-021-03879-8 [Crossref] [ Google Scholar]
- Shori T, Kolte A, Kher V, Dharamthok S, Shrirao T. A comparative evaluation of the effectiveness of subpedicle acellular dermal matrix allograft with subepithelial connective tissue graft in the treatment of isolated marginal tissue recession: a clinical study. J Indian Soc Periodontol 2013; 17(1):78-81. doi: 10.4103/0972-124x.107479 [Crossref] [ Google Scholar]
- Sumana SZ, Lelyati S, Lessang R. Root coverage using the subepithelial connective tissue graft or the acellular dermal matrix for the treatment of gingival recession: a clinical study. Int J Appl Pharm 2017; 9(2):20-3. doi: 10.22159/ijap.2017.v9s2.06 [Crossref] [ Google Scholar]
- Taiyeb Ali TB, Shapeen IM, Ahmed HB, Javed F. Efficacy of acellular dermal matrix and autogenous connective tissue grafts in the treatment of gingival recession defects among Asians. J Investig Clin Dent 2015; 6(2):125-32. doi: 10.1111/jicd.12085 [Crossref] [ Google Scholar]
- Vincent-Bugnas S, Laurent J, Naman E, Charbit M, Borie G. Treatment of multiple gingival recessions with xenogeneic acellular dermal matrix compared to connective tissue graft: a randomized split-mouth clinical trial. J Periodontal Implant Sci 2021; 51(2):77-87. doi: 10.5051/jpis.2002400120 [Crossref] [ Google Scholar]
- Chambrone L, Ortega MAS, Sukekava F, Rotundo R, Kalemaj Z, Buti J. Root coverage procedures for treating single and multiple recession-type defects: an updated Cochrane systematic review. J Periodontol 2019; 90(12):1399-422. doi: 10.1002/jper.19-0079 [Crossref] [ Google Scholar]
- Neiva R, Giannobile WV. Mucosal and gingival tissue engineering. In: Ferri J, Hunziker EB, eds. Preprosthetic and Maxillofacial Surgery. Woodhead Publishing; 2011. p. 305-26. 10.1533/9780857092427.3.305
- Ayub LG, Ramos UD, Reino DM, Grisi MF, Taba M Jr, Souza SL. A Randomized comparative clinical study of two surgical procedures to improve root coverage with the acellular dermal matrix graft. J Clin Periodontol 2012; 39(9):871-8. doi: 10.1111/j.1600-051X.2012.01915.x [Crossref] [ Google Scholar]
- Karring T, Lang NP, Löe H. The role of gingival connective tissue in determining epithelial differentiation. J Periodontal Res 1975; 10(1):1-11. doi: 10.1111/j.1600-0765.1975.tb00001.x [Crossref] [ Google Scholar]
- Owens JL, Cordell KG, Amornporncharoen M, Palaiologou AA. Histologic evaluation of acellular dermal matrix allografts in humans. Clin Adv Periodontics 2017; 7(3):122-7. doi: 10.1902/cap.2017.160057 [Crossref] [ Google Scholar]
- Wang HL, Romanos GE, Geurs NC, Sullivan A, Suárez-López Del Amo F, Eber RM. Comparison of two differently processed acellular dermal matrix products for root coverage procedures: a prospective, randomized multicenter study. J Periodontol 2014; 85(12):1693-701. doi: 10.1902/jop.2014.140198 [Crossref] [ Google Scholar]
- Silc JT, Petrungaro PS. Acellular dermal matrix grafts for root coverage procedures: review of products and introduction of a new technique. Compend Contin Educ Dent 2013; 34(6):408-14. [ Google Scholar]
- Wei PC, Laurell L, Geivelis M, Lingen MW, Maddalozzo D. Acellular dermal matrix allografts to achieve increased attached gingiva. Part 1. A clinical study. J Periodontol 2000; 71(8):1297-305. doi: 10.1902/jop.2000.71.8.1297 [Crossref] [ Google Scholar]
- Chambrone L, Sukekava F, Araújo MG, Pustiglioni FE, Chambrone LA, Lima LA. Root-coverage procedures for the treatment of localized recession-type defects: a Cochrane systematic review. J Periodontol 2010; 81(4):452-78. doi: 10.1902/jop.2010.090540 [Crossref] [ Google Scholar]
- Harris RJ. A short-term and long-term comparison of root coverage with an acellular dermal matrix and a subepithelial graft. J Periodontol 2004; 75(5):734-43. doi: 10.1902/jop.2004.75.5.734 [Crossref] [ Google Scholar]