J Adv Periodontol Implant Dent. 17(1):15-25.
doi: 10.34172/japid.2025.002
Original Article
Clinical effectiveness of aloe vera gel as an adjunct to mechanical debridement in patients with periodontitis: A systematic review and meta-analysis
Nisha Ashifa Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Visualization, Writing – original draft, Writing – review & editing, 1, * 
Krishnan Viswanathan Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Writing – review & editing, 1 
Sivapragasam Srinivasan Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Writing – review & editing, 1 
Varsha K. Pavithran Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, 2 
Shiva Shankar Formal analysis, Investigation, Methodology, Project administration, Software, Validation, Visualization, Writing – original draft, Writing – review & editing, 3 
Rajasekar Sundaram Methodology, Project administration, Supervision, Writing – review & editing, 1 
Senthil Kumar Methodology, Project administration, Supervision, Writing – review & editing, 1
Divvi Anusha Formal analysis, Investigation, Methodology, Project administration, Software, Validation, Writing – original draft, Writing – review & editing, 3 
Author information:
1Department of Periodontology, Rajah Muthiah Dental College & Hospital, Annamalai University, Annamalai Nagar, Tamil Nadu, India
2Public Health Researcher & Biostatistician, Rypple Foundation Cypresstraat 64, 2565LW Den Haag, India
3Department of Public Health Dentistry, Indira Gandhi Institute of Dental Sciences, Sri Balaji Vidyapeeth, Puducherry, India
Abstract
Background.
This study aimed to evaluate the clinical effect of aloe vera gel as an adjunct to scaling and root planing (SRP) on plaque index (PI), gingival index (GI), and probing pocket depth (PPD) in periodontitis treatment.
Methods.
Randomized controlled trials (RCTs) were included, focusing on aloe vera gel as an adjunct to SRP in periodontitis patients. An extensive literature search was conducted across PubMed, PubMed Central, Scopus, OVID, Google Scholar, and Cochrane Library databases up to October 2024. The risk of bias was assessed using the Revised Cochrane Risk of Bias tool (ROB 2.0), and statistical analysis was performed using Review Manager 5.4.1.
Results.
Fifteen RCTs were included in this systematic review, and separate meta-analyses were conducted for each outcome. For PI, the random effects model showed a mean difference (MD) of -0.23 (95% CI: -0.69, 0.23), favoring the experimental group (P=0.33). The fixed effects model for PI favored the control group (MD=0.12; P=0.20). For GI, the random effects model favored the experimental group (MD=-0.28, P=0.01), while the fixed effects model favored the control group (MD=0.17; P<0.001). For PPD, the random effects model favored the experimental group (MD=-0.45, P=0.009).
Conclusion.
As an adjunct to SRP, aloe vera gel significantly improved PI, GI, and PPD in periodontitis patients.
Trial registration.
PROSPERO ID: CRD42020201315.
Keywords: Aloe vera gel, Dental scaling, Meta-analysis, Periodontitis, Root planing, Systematic review
Copyright and License Information
© 2025 The Author(s).
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Funding Statement
This research received no specific grant from funding agencies in
the public, commercial, or not-for-profit sectors.
Introduction
Periodontitis is a globally prevalent oral disease affecting the periodontium. It presents with gingival inflammation, connective tissue degradation, and alveolar bone loss, eventually leading to tooth loss. The complex interaction between the pathobionts and the host immune response is responsible for the disease’s commencement and progression.1,2
Periodontal treatment is primarily concerned with reducing the burden of pathogenic subgingival bacteria and resolving inflammation.2-4 The initial step in periodontal treatment is the nonsurgical management, which consists of mechanical debridement, supra- and sub-gingival irrigation, and the use of additional chemotherapeutic agents.2,3 Mechanical debridement refers to scaling and root planing (SRP), which is the elimination of supragingival and subgingival deposits using hand and/or power-driven instruments. Thus, SRP helps restore periodontal health by reducing microbial load.2,5,6
Various treatment options are being used secondary to SRP, including systemic and locally applied antimicrobial agents, antiseptics, anti-inflammatory agents, and nonsurgical use of lasers.5,7 These adjunctive aids enhance the effects of SRP and promote healing. Systemic and local antimicrobial agents have been widely used. However, these agents are associated with adverse effects like antimicrobial resistance, gastrointestinal intolerance, altered taste sensation, staining of teeth, and many more.8-11 Recently, phytotherapeutic agents have garnered significant attention as supplementary treatments to nonsurgical periodontal therapy due to their positive qualities like availability, good patient tolerance, reduced cost, and reduced side effects.8,12
Aloe vera, botanically known as Aloe barbadensis, is a highly valued medicinal plant from the family Liliaceae. It is widely recognized for its wound healing, anti-inflammatory, immunomodulatory, antimicrobial, and antioxidant properties. It also stimulates epithelial cell migration and collagen maturation, promoting tissue regeneration.13,14 It is used to treat wounds, burns, skin disorders, infections, gastrointestinal disorders, hemorrhoids, hair loss, and sinusitis.13,15,16 In dentistry, aloe vera is used as a topical applicant for oral lesions like aphthous ulcers, oral lichen planus, pemphigus, angular cheilitis, herpetic lesions, oral submucous fibrosis, traumatized tissues, on extraction sockets, chemical burns, in denture stomatitis and periodontally infected sites.13,17
The pharmacological qualities of aloe vera make it valuable for the treatment of periodontitis.13,14,17 When used as a mouthwash, aloe vera exhibits optimistic results in resolving gingival inflammation, with no documented side effects.15 In patients with periodontitis, subgingival placement of aloe vera gel or chip significantly improved clinical parameters.5,13,18-20 Singh et al.20 found a significantly higher level of antioxidant levels in GCF after applying aloe vera gel to periodontitis patients.
In today’s world, clinicians are expected to keep pace with advancements in knowledge and clinical practice. Evidence-based practice is the application of research findings into clinical practice. Considering the usefulness of aloe vera in treating periodontal diseases, the present systematic review/meta-analysis addresses the question, “What is the effectiveness of aloe vera gel used as an adjunct to mechanical debridement in the treatment of periodontitis, when compared to SRP alone or with placebo?”
Methods
Registration and protocol
The study protocol was registered at PROSPERO International Prospective Register of Systematic Reviews (ID: CRD42020201315). This systematic review and meta-analysis were prepared in accordance with Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines21 and the Cochrane Handbook of Systematic Reviews and Interventions.22
Focused question
The present study focuses on the question, “What is the effectiveness of aloe vera gel used as an adjunct to SRP in the treatment of periodontitis when compared to SRP alone or with a placebo?”
Eligibility criteria
A PICO-based search strategy was developed as follows.
Study characteristics in PICO format
Randomized controlled trials (RCTs) were included in this study.
Participants (P): Patients with periodontitis with a probing pocket depth (PPD) of 4‒8 mm
Intervention (I): Subgingival administration of aloe vera gel as an adjunct to SRP
Comparison (C): With SRP alone or with a placebo
Outcome (O): Plaque index (PI), gingival index (GI), PPD
Inclusion criteria
-
RCTs done on patients with periodontitis with a PPD of 4‒8 mm
-
RCTs done with aloe vera gel as an adjunct to SRP with 4‒6 weeks of follow-up
-
No restrictions on age and gender
-
Full-text articles
-
RCTs published until October 2024
-
Articles published in the English language
Exclusion criteria
-
Studies using aloe vera in any other form were not considered.
-
Non-randomized trials (controlled/uncontrolled), case series, case reports, descriptive and analytical studies, in vitro studies, animal studies, review papers, letters to the editor, monographs, and conference papers were excluded.
-
Literature in other languages that could not be translated by the reviewer was excluded.
-
Unpublished data with full access.
Information sources
An extensive electronic search was conducted on PubMed/MEDLINE, PubMed Central, OVID, Google Scholar, and Cochrane Library databases up to October 2024 to determine the eligible studies for this review. Further studies were found by hand-searching the reference lists of the selected papers.
Search terms used ( MeSH terms)
The search terms used to identify relevant articles were periodontitis, adult periodontitis, chronic periodontitis, aloe vera gel, aloe, scaling, dental, supragingival, supragingival scaling and root scaling, root planing, planing, nonsurgical periodontal therapy, local drug therapy, local drug delivery, local drug delivery (LDD), outcome, treatment, patient-relevant outcome, clinical effectiveness, treatment effectiveness, rehabilitation outcome, outcome, rehabilitation, effectiveness.
Study selection process
Two reviewers (NA and KV) independently examined the titles and abstracts of all studies during the preliminary round of study selection. A third author (RS) was brought in to settle the differences over the eligibility of the articles. Irrelevant studies were excluded. The full texts of the articles that met the inclusion criteria and the keywords were gathered. Further screening of the full texts of the selected articles was performed during the second round of the study selection. Articles that did not match the inclusion criteria were excluded from consideration, and the reasons for exclusion were noted (Table 1).
Data collection process and data items
Data from the chosen articles were collected by two reviewers (NA and KV) using data extraction forms, which included details like the details of the study, year of publication, study design, participants and grouping, intervention and comparison, number of applications of aloe vera gel, parameters assessed, follow-up, statistical analysis used, and outcome. A third reviewer (SK) settled the disagreements over the data to be extracted.
Risk of bias assessment
Two reviewers (NA and SS) used the ROB2.0 tool to evaluate the risk of bias in the included RCTs, adhering to the Revised Cochrane Risk of Bias guidelines.42 This instrument consists of five items, which include bias due to randomization, deviation from intended intervention, missing outcome data, measurement of the outcome, and selection of the reported result. The articles were deemed low risk if all the criteria were met, high risk if one or more criteria were not met, and some concerns of bias if one or more criteria were partly met or had insufficient information. Finally, the overall bias for each article was also assessed. Disagreements regarding the same were settled by a third reviewer (VKP).
Effect measures and synthesis of results
Data on the outcomes were extracted from each study and initially entered into Microsoft Excel. The statistical analysis was conducted using the licensed Review Manager version 5.4.1 [Review Manager ( RevMan ) [Computer program]. Version 5.4. The Cochrane Collaboration, 2020. The chi-squared test and I2test were used to calculate the heterogeneity between the studies. An inverse variance statistical method along with random effects analysis model was employed for an expected outcome of continuous data type, and the effects estimate measure was expressed as mean difference (MD) with totals, subtotals, and 95% confidence interval. The pooled effect measure (overall effect) was estimated using the Z test. The level of significance was determined at P ≤ 0.05. Forest plots and funnel plots were created for graphical presentations of results.
Results
Study selection
A total of 1727 articles were found in the search results (1709 from databases and 18 from additional sources). After removing duplicates, 1438 articles were screened for the titles and abstracts. Following screening, 1401 articles were eliminated, and 37 articles were retained. The full texts of these 37 articles were reviewed, and 22 articles were excluded. Finally, 15 articles were included in the systematic review.1,5,18,20,43-53 Out of these 15 articles, six articles18,45,48,50,51,53 were used for the meta-analysis of mean PI, two49,51 were used for meta-analysis of mean change in PI, seven articles18,45,46,48,50,51,53 were used for the meta-analysis of mean GI, two49,51 were used for meta-analysis of mean change in GI, and eight articles18,20,45,46,48,50,51,53 were used for meta-analysis of PPD (Figure 1). An overview of the articles that were excluded is provided in Table 1.
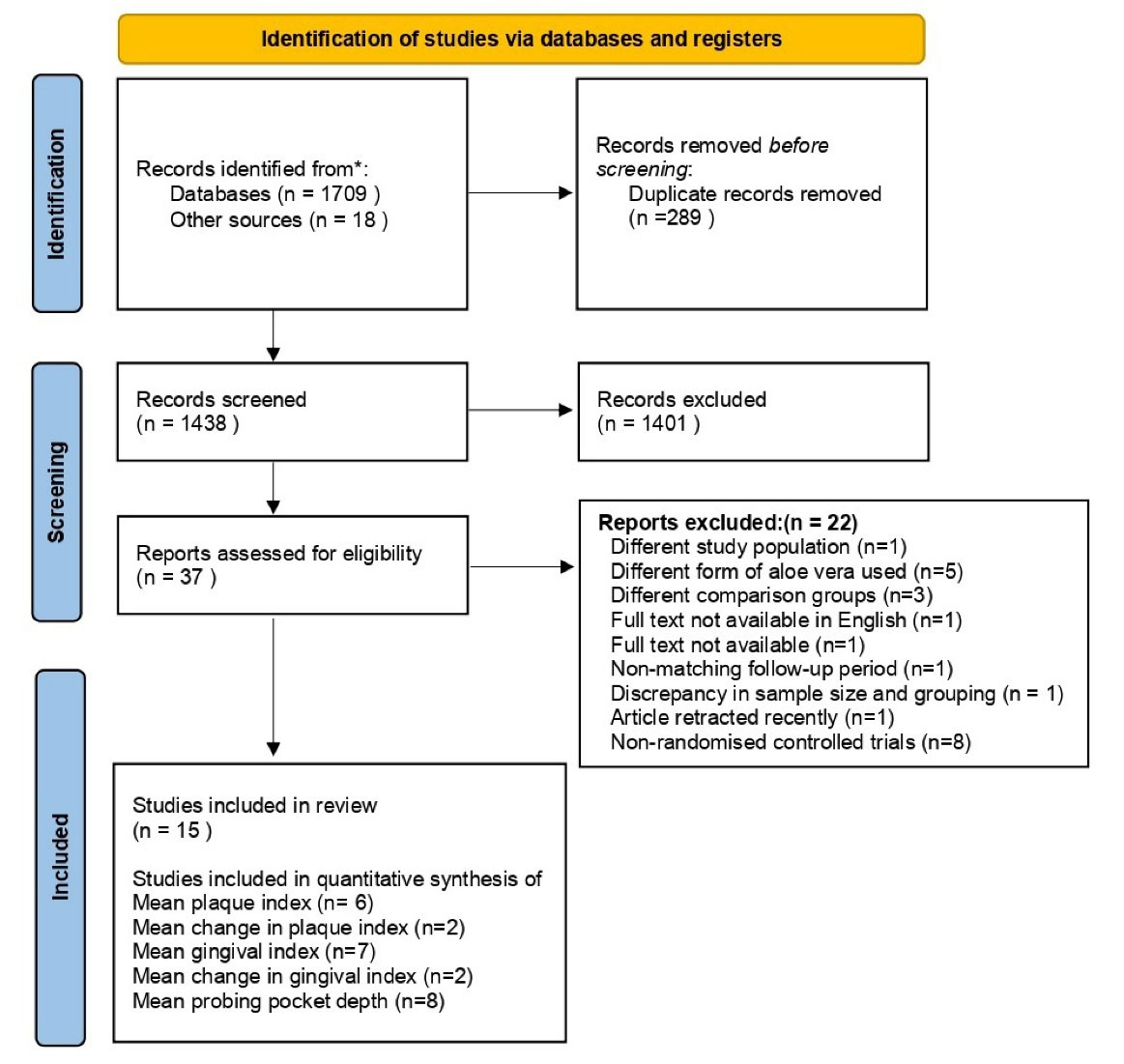
Figure 1.
PRISMA flow diagram 2020. PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-analysis
.
PRISMA flow diagram 2020. PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-analysis
Table 1.
Excluded studies and the reasons for exclusion
|
Author, Year
|
Reason
|
Pradeep et al, 2016 14
(n = 1) |
Conducted the study in patients with Type 2 diabetes mellitus |
Rathod et al, 2015 19
Rithesh K 202123
(n = 2) |
Used aloe vera chip as an adjunct to SRP |
Choudhary et al, 202024
(n = 1) |
Used Aloin (aloe vera extract) as an adjunct to SRP |
Gupta et al, 202125
(n = 1) |
Implemented subgingival irrigation of aloe vera, and the outcome was compared with chlorhexidine irrigation |
Sharma et al. 201826
(n = 1) |
The effect of aloe vera gel was compared with probiotic lozenges |
Sahgal et al, 201527
(n = 1) |
The follow-up period of the study is 7 days |
Penmetsa et al, 201928
(n = 1) |
The effect of aloe vera as an adjunct was compared with 1% Ornidazole and 0.25% chlorhexidine gluconate gel |
Kumar et al, 201529
(n = 1) |
The effect of aloe vera gel is compared with propolis gel |
Hermanto et al, 201530
(n = 1) |
Full text not available in English |
Bommireddy et al, 202331
(n = 1) |
Full text not available. Abstract published in Special Edition of 2023 FDI World Dental Congress |
Sayar et al, 202132
(n = 1) |
Used aloe vera toothpaste |
Elsadek et al, 202033
(n = 1) |
Article retracted recently |
Vijay et al, 202234
(n = 1) |
Discrepancy in the sample size and grouping |
Bhat et al, 201113
Dodwad and Arora 201135
Abdelmonem et al, 201436
Sangwan et al, 201737
Nazir & Kumar, 201838
Phatale & Chavda, 202039
Timothy & Rajasekar, 202040
Katariya & Rajasekar, 202441
(n = 8) |
Non-randomized clinical trials |
Study characteristics
This study analyzed 15 RCTs.1,5,49–53,18,20,43-48 All these studies evaluated the clinical efficacy of subgingival placement of aloe vera gel as an adjunct to SRP in patients with periodontitis. Participants in the test group received SRP + aloe vera gel, whereas the control group received SRP or SRP plus a placebo gel. Table 2 presents the characteristics of the included studies. Out of 15 trials that were included, 11 trials reported a single application of aloe vera following SRP,1,5,53,18,20,43,45-47,51,52 while four reported multiple applications.44,48-50 Two RCTs used Curagel (by Cure Pharma),48,49 two RCTs used 98% aloe vera gel,5,18 one RCT used 2.5% aloe vera gel,51 and one RCT used 99% aloe vera gel.45 The follow-up time in all trials ranged from 3 weeks to 12 months.
Table 2.
Characteristics of the studies included in the systematic review
|
Study and year
|
Study design
|
Participants & group
|
Intervention & comparison
|
Number of applications of Aloe vera gel
|
Parameters assessed
|
Follow-Up
|
Statistical analysis used
|
Outcome
|
| Virdi et al, 201248 |
Split-mouth, randomized controlled study |
20 patients divided into test and control group |
SRP only + Aloe vera gel vs SRP only |
Multiple applications at
Baseline
1st week
2nd week |
PI
GI
PPD |
6 weeks |
Paired t-test,
ANOVA |
The intragroup comparison revealed a statistically significant difference in PI, GI, and PPD scores. On intergroup comparison, a statistically significant difference was present in the GI and PPD scores but not in PI scores at 6 weeks. |
| Sethi et al, 201518 |
Split-mouth,
Randomized controlled study |
10 patients, each with at least 3 sites in different quadrants, were included. |
SRP only + Aloe vera gel vs SRP only |
Single application – at baseline |
PI
GI
PPD |
3 weeks
6 weeks |
paired t-test,
one way ANOVA,
Post-hoc Turkey’s test,
Kruskal Wallis ANOVA,
Mann-Whitney test,
Fisher’s exact test. |
On intra-group analysis, there was a significant reduction (P < 0.01) of PI, GI, and PPD & in all the treatment groups. On intergroup analysis, no significant difference was observed across groups at 3 and 6 weeks. |
| Singh et al, 201649 |
Split-mouth,
Randomized controlled study |
60 sites from 20 patients, out of which 40 sites were
test sites, and 20 sites were control sites |
SRP + Aloe vera gel (Curagel) vs SRP |
Multiple applications – at
Baseline
7th day |
PI
GI
PPD |
30 days
60 days
90 days |
Paired t-test, ANOVA |
On intergroup comparison, scores of PI and GI were statistically significant (P < 0.05), but PPD was not statistically significant (P = 0.15) |
| Moghaddam et al, 20175 |
Split-mouth, randomized clinical trial |
20 patients divided into test and control sites |
SRP vs SRP + 98% Aloe vera gel |
Single application – at baseline |
PI
GI
PPD |
30th day
60th day |
Repeated ANOVA measures,
independent test,
Kolmogrov-Smirnov test |
On intergroup comparison, differences in PI, GI, and PPD on the 30th and 60th day between the cases and control group were statistically significant. |
| Dilliwal et al, 201750 |
Split-mouth,
randomized controlled clinical trial |
30 sites from 15 patients divided into 2 groups – Group I and II |
SRP + Aloe vera gel vs SRP only |
Multiple applications at
Baseline
7th day
15th day |
PI
GI
PPD |
30 days |
Friedman test,
Wilcoxon signed-rank test,
Mann-Whitney U test |
Both intragroup and intergroup comparisons revealed that the mean PI, GI, and PPD were statistically significant on day 30 |
| Deepu et al, 201851 |
RCT |
Total 71 patients divided into 2 groups:
Test group -33 Control group -38
Total Sites: 266
Test group: 122
Control Group: 144 |
SRP + 2.5% Aloe vera gel vs SRP + Placebo gel |
Single application – at baseline |
PI
GI
PPD |
1 month
2 months
4 months |
Independent t-test |
A statistically significant difference in PPD and GI was observed in the test group compared to the control group in the 1st month but not in 2nd and 4th month. However, a significant difference in PI was noted for both groups in the 2nd month but not in 1 and 4 months. |
| Ipshita et al, 20181 |
Single-center, randomized, controlled clinical trial |
30 patients in each test and control group |
SRP + placebo gel LDD vs SRP + Aloe vera gel LDD |
Single application – at baseline |
PI
PPD |
6 months
12 months |
Mean ± standard deviation,
one-way ANOVA,
Scheffe’s post hoc tests,
repeated measures ANOVA |
The mean PI scores were not statistically significant; however, the mean PPD scores showed a statistically significant difference at 6 months and 12 months |
| Kurian et al, 201852 |
Randomized, single-center, longitudinal,
parallel-arm design study |
30 patients in each test and control group |
SRP + placebo gel
vs SRP + 1% Aloe vera gel |
Single application – at baseline |
PI
PPD |
6 months
12 months |
Mean ± standard deviation,
one-way ANOVA,
Scheffe’s post hoc tests,
repeated measures ANOVA |
The mean PI scores were not statistically significant, but there was a statistically significant difference in the mean PPD scores at 6 months and 12 months |
| Agrawal et al, 201953 |
Split-mouth, randomized controlled study |
40 sites from 20 subjects divided into a test group and a control group |
SRP + Aloe vera gel
vs SRP only |
Single application – at baseline |
PI
GI
PPD |
1 month |
Paired t-test, independent t-test |
The intragroup comparison revealed a statistically significant reduction in the mean PI, GI, and PPD 1 month in both groups (P < 0.001). On intergroup comparison, a statistically significant difference in PPD between the groups at 1 month (P < 0.05) |
| Singh et al, 201920 |
Split-mouth randomized controlled study |
30 subjects |
SRP + 80% Aloe vera gel vs SRP only |
Single application – at baseline |
PPD |
1month |
Student’s t-test, repeated ANOVA |
No statistical significance was observed in PPD between the test and control group at baseline and 1-month follow-up |
| Qamar et al, 202143 |
Randomized controlled study |
50 patients in each test group and control group |
SRP vs SRP + Aloe vera gel |
Single application – at baseline |
PI
PPD |
3 months
6 months |
Kruskal- Wallis test,
Bonferroni`s post-hoc test |
Statistically significant improvement was noted for PI and PPD in the test group at follow-up, compared to the control group. |
| Tayeb et al, 202244 |
RCT |
15 patients in the test group and 15 patients in the control group |
SRP + Aloe vera gel vs SRP only |
Multiple applications – at
Baseline
1st week
2nd week |
GI
PPD |
3 months
6 months
9 months |
ANOVA test,
Friedman test,
Bonferroni’s post hoc test |
AV group showed a statistically significant reduction in PD compared to the control group at 3, 6, and 9 months. With respect to GI, a statistically significant difference was noted at 6 months and 9 months follow-up, but not at 3 months follow-up. |
| Borgohain et al, 202345 |
Split-mouth randomized controlled study |
10 patients |
SRP vs
SRP + 99% Aloe vera gel |
Single application – at baseline |
PI
GI
PPD |
30days |
Not mentioned |
The intergroup comparison between the test and the control group for all parameters at baseline and on the 30th day after the intervention revealed statistically significant differences in terms of PPD and GI. |
| Faramarzi et al, 202446 |
Double-blind randomized split-mouth study |
20 patients |
SRP vs SRP + Aloe vera gel |
Single application – at baseline |
GI
PPD |
30days |
Kolmogorov-Smirnov test,
paired t-test, independent t test |
A significant difference was noted between the test and the control group at 30 days follow-up |
| Marella et al, 202447 |
Single-blind randomized split-mouth study |
20 patients |
SRP vs SRP + Aloe vera gel |
Single application – at baseline |
PI
PPD |
3 months |
Mann–Whitney U test, Wilcoxon signed-rank test, chi-squared test, McNemar’s test |
The significant differences observed between the test and control groups in PI and PPD parameters at three months, with no notable differences at baseline, confirm the greater beneficial effect of the intervention in the test group. |
Abbreviations: ANOVA: analysis of variance, GI: gingival index, PI: plaque index, PPD: probing pocket depth, SRP: scaling and root planing; RCT: Randomized controlled trial.
Risk of bias assessment
The graphs for ROB2.0 were generated using Robvis.54The domain-level judgments for each study in the Traffic light plot (Figure 2) showed that three studies had a low overall risk of bias, four studies had some concerns, and eight studies had a high overall risk of bias. The distribution of risk-of-bias judgments within each bias domain in the Summary bar plot (Figure 3) depicted a 20% low bias, 27% unclear bias, and 53% high overall risk of bias. The lowest risk was observed in the three main areas of conducting an RCT – missing outcome data (100%), deviations from intended interventions (67%), and randomization process (67%), thus assuring the strength of the methodology of the included studies. However, the highest risk was observed in the measurement outcome (48%) due to the inconsistencies in the measurement of the outcome variable using other indices and non-blinding of investigators
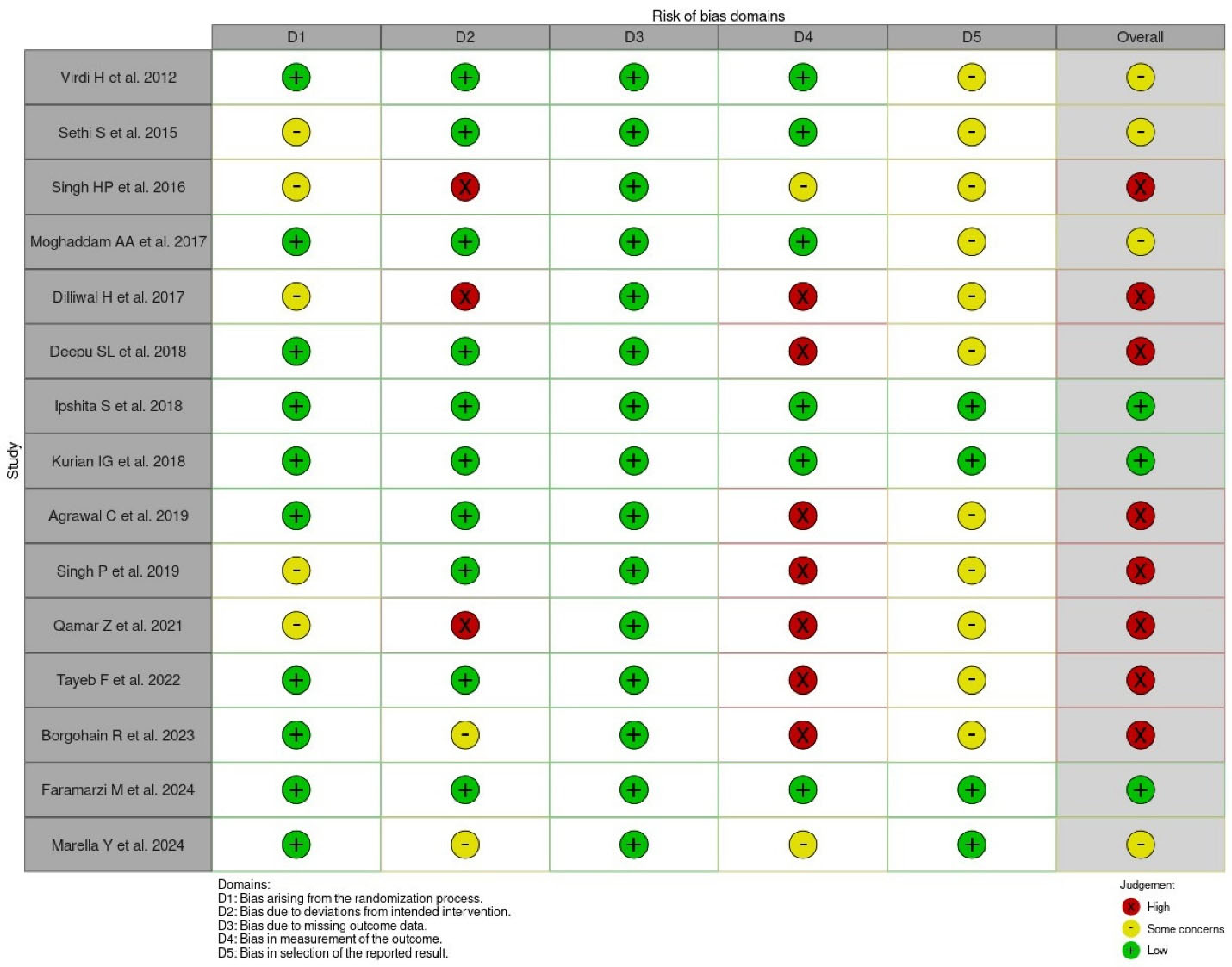
Figure 2.
Traffic-light plot of ROB 2.0 assessment of the included studies
.
Traffic-light plot of ROB 2.0 assessment of the included studies
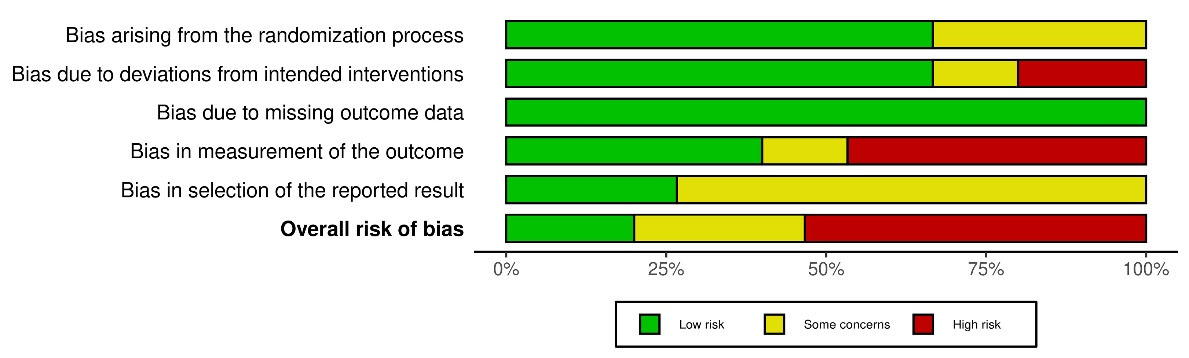
Figure 3.
Summary bar plot of ROB 2.0 assessment of the included studies
.
Summary bar plot of ROB 2.0 assessment of the included studies
Meta-analysis of PI
Mean PI (random effects model)
The pooled MD in a random model analysis of PI on teeth at 4‒6 weeks post-intervention was -0.23 (pooled 95% CI: -0.69, 0.23; P = 0.33), favoring the experimental group. Out of the total 6 studies included in the meta-analysis of PI, three studies45,48,50 showed MD of PI favoring the experimental group (aloe vera + SRP), two studies18,53 showed no MD, and one study51 favored the control group (SRP alone), all with narrower 95% CI. The treatment (aloe vera adjunct to mechanical debridement) in periodontitis patients had a 50% effect on reducing PI scores in 4‒6 weeks. The I2 statistic of PI on teeth post-intervention showed significant heterogeneity of 97% (Tau2 = 0.31; χ2 = 157.79, df = 5, P < 0.00001). The test for overall effect non-significantly favored the experimental group (Z = 0.98; P = 0.33) (Figure 4).
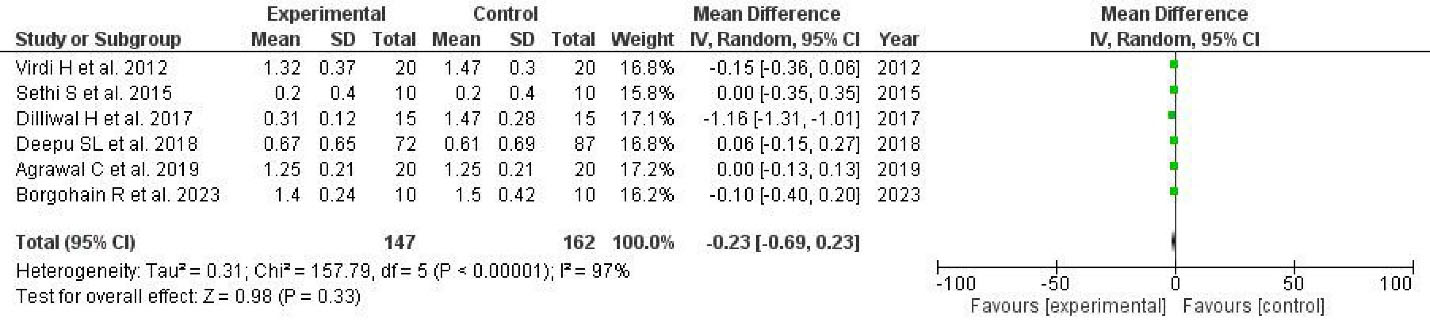
Figure 4.
Forest plot of the mean plaque index
.
Forest plot of the mean plaque index
Mean changes in PI (fixed effects model)
The fixed effects model showed an increased PI (MD = 0.12; 95% CI: 0.09, 0.15; P = 0.20, not significant) at 1 month, favoring the control group, with the I2 statistic showing moderate heterogeneity (40%) (Figure 5).
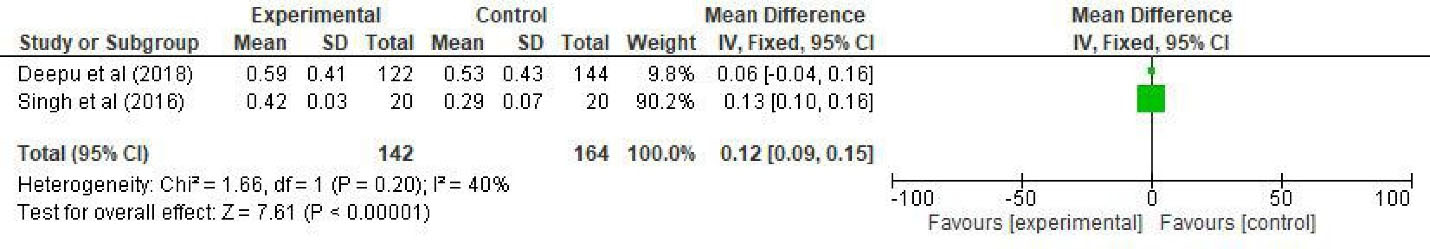
Figure 5.
Forest plot of mean changes in plaque index
.
Forest plot of mean changes in plaque index
Meta-analysis of GI
Mean GI (random effects model)
A significant pooled mean difference in the GI of teeth post-intervention (4‒6 weeks) was observed in a random model analysis. The overall effect was -0.28 (pooled 95% CI: -0.51, -0.60), favoring the experimental group (Z = 2.48; P = 0.01). Among the 7 studies used for the meta-analysis of the GI, five studies45,46,48,50,51 favored the experimental group, and two studies18,53 had no MD, with a considerably broader 95% CI compared to the PI analysis. The treatment for periodontitis patients using aloe vera as an adjunct to mechanical debridement showed a 71% effect on reduction in the GI scores in 4‒6 weeks. The heterogeneity test showed the I2 statistic of the GI to be significant with 92% heterogeneity (Tau2 = 0.07; χ2 = 76.79, df = 6, P < 0.00001) (Figure 6).
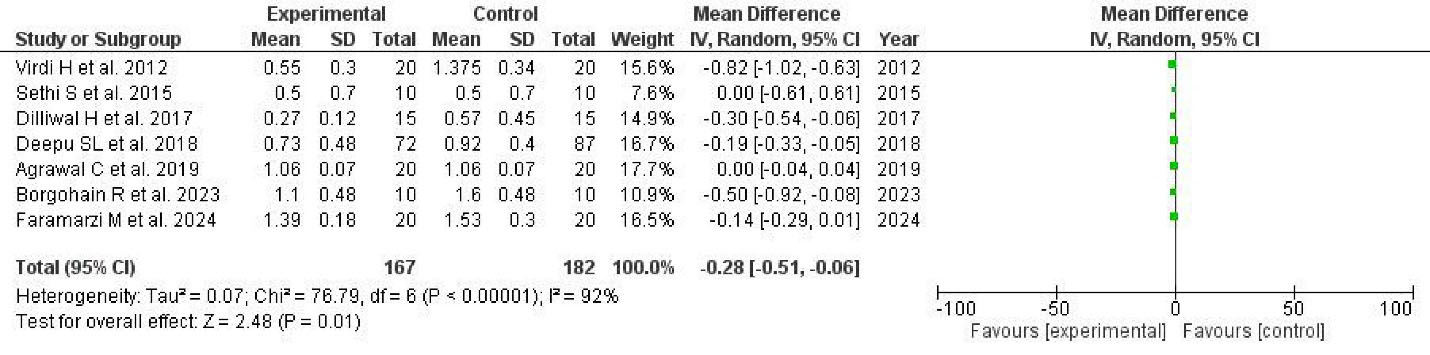
Figure 6.
Forest plot of the mean gingival index
.
Forest plot of the mean gingival index
Mean changes in GI (fixed effects model)
The fixed effects model showed an increased GI (MD: 0.17; 95% CI: 0.12, 0.23; P = 0.00001, significant) at 1 month, favoring the control group, with the I2 statistic showing zero heterogeneity (0%).
Meta-analysis of PPD
Mean PPD
A significant pooled mean difference in a random model analysis of PPD on teeth at 4‒6 weeks post-intervention was -0.45 (pooled 95% CI: -0.78, -0.11), favoring the experimental group (Z = 2.63; P = 0.009). Out of the total 8 studies included for the meta-analysis of PPD, seven studies20,45,46,48,50,51,53 showed MD of PPD, favoring the experimental group, and one study18 favored the control group, all with a broader 95% CI. The use of aloe vera and mechanical debridement in periodontitis patients showed an 88% effect in reducing the PPD levels after 4‒6 weeks. The I2 statistic of PPD post-intervention showed a significant heterogeneity of 84% (Tau2 = 0.16; χ2 = 42.78, df = 7, P < 0.00001).
Mean change in PPD
Only one eligible study reported a significant mean change in PPD between the test and control groups; hence, a meta-analysis was not conducted.51
Publication bias
A funnel plot was prepared to assess the publication bias in all the studies included in the meta-analysis. The plotting consists of an effect estimate (mean difference) on the X-axis and a standard error of the mean difference on the Y-axis. Each circle represents the individual study effect estimate. Aggregation of individual study effect estimates was observed to coincide with the overall effect estimate line (middle line) and well within the 95% CI of the funnel, representing the majority of the larger precision studies on the top of the funnel as depicted in the GI and no publication bias. The funnel plots of PI and PPD had most of the studies plotted on the middle and lower section of the funnel, suggesting lower precision, indicating no publication bias in the current meta-analysis.
Discussion
Aloe vera is a medicinal plant renowned for its diverse therapeutic properties, including promoting wound healing, providing pain relief, reducing inflammation, and exhibiting antibacterial, antifungal, antiviral, antioxidant, and immunomodulatory properties.55 It also offers protection against radiation-induced mucositis and lowers the likelihood of oral thrush in patients receiving radiotherapy.56 Aloe vera has various applications due to its medicinal properties in periodontics. In 2014, Dhingra, in his systematic review, concluded that, although the studies included reported the aloe vera dentifrices to be equally effective as conventional dentifrices, the outcomes could not be conclusively reported due to the significant risk of bias of the studies.57 Another systematic review by Al-Maweri et al15 stated that aloe vera mouthrinse was equally effective as chlorhexidine in minimizing gingival inflammation and less effective than chlorhexidine in minimizing plaque. Recently, Jadhav et al58 reported that locally delivered aloe vera significantly improved periodontal parameters.
The current systematic review focuses on the question, “What is the clinical effectiveness of the subgingival application of aloe vera gel as an adjunct to SRP in the treatment of periodontitis?”
RCTs available on different databases until October 2024 were included in this review, as they are categorized as Level II evidence in the hierarchy. An extensive literature search was conducted, and 15 RCTs that fulfilled the eligibility criteria were chosen for this study.
The current systematic review summarizes the fifteen studies included; fourteen1,5,50-53,20,43-49 studies indicated that using aloe vera gel along with SRP proved to be advantageous in the treatment of periodontitis, whereas one study18 reported no difference between the two groups. Deepu et al51 found that aloe vera gel was effective in the short term (one-month follow-up) but had no effect in the long term (two-month and four-month follow-ups). There were no reported side effects from using aloe vera gel in any of these studies. In all these trials, aloe vera was injected into the periodontal pocket after SRP in the test group.
The primary outcomes assessed in this study were PI, GI, and PPD. This meta-analysis demonstrated that adjunctive use of aloe vera gel with SRP significantly enhanced PI, GI, and PPD in patients with periodontitis. The antiplaque activity of aloe vera can be credited to its antibacterial and antifungal action, especially against Streptococcus and Candida species.15,59 Numerous pharmacologically active substances found in aloe species, including homonataloin, aloeresin, aloe emodin, aloin (the C-glucoside of aloe emodin), and chrysophanol, have all been linked to its antimicrobial activity.60 The anti-gingivitis effect of aloe vera can be linked to its antiplaque and potent anti-inflammatory characteristics.15 Aloe extracts are effective against bradykinin, histidine, COX-1, and COX-2 enzymes.60 Additionally, aloe vera includes elements that aid in forming collagen, including vitamin C, mannose-6-phosphate, dermatan sulfate, and hyaluronic acid, which reduce swelling and gingival bleeding.15,59 Aloins can inhibit matrix metalloproteinases (MMPs) because they are structurally analogous to tetracyclines.61 Inhibition of MMP-2 and MMP-9 prevents tissue destruction in periodontitis.62 Furthermore, aloins inhibit collagenase activity and stimulate cell development, producing greater collagen content.61 As a result of these properties, aloe vera improves the PPD.
The meta-analysis of all three parameters revealed a sizable heterogeneity, which might be attributed to the limitations of clear evidence. Lack of standardization and intra-examiner calibration were noted in most of the studies included in this meta-analysis. Additionally, we encountered inconsistencies in the number of applications and the concentration of aloe vera gel used in these studies. Regrettably, no literature is available on the sustenance and half-life of aloe vera gel when placed in the periodontal pocket. Hence, the substantivity and bio-availability of aloe vera gel cannot be debated. However, Sethi et al18 proposed using a bio-adhesive compound with aloe vera gel to keep it in the periodontal pocket for a longer period for greater advantages. The use of aloe vera gel with different concentrations may also have influenced the results of this meta-analysis. Furthermore, as the included studies published their results in different formats, separate analyses were performed for studies with mean and standard deviation data and studies with mean change data. Also, inadequacy in the total number of studies included with language specificity (English) seems to be another drawback.
Conclusion
The findings of this study indicate that the adjunctive use of aloe vera gel effectively reduces PI, GI, and PPD in patients with periodontitis, with no adverse effects observed. Based on these results, it is recommended that future research include long-term clinical trials with standardized methodologies to provide more robust evidence on the efficacy of aloe vera gel in periodontal treatment.
Competing Interests
The authors declare that they have no competing interests.
Data Availability Statement
The study protocol, methodology, search terms used, and statistical analysis plan have been discussed in the manuscript.
Ethical Approval
Not applicable.
Acknowledgements
We would like to express our gratitude to the Library and Department of Periodontology, Rajah Muthiah Dental College and Hospital, Annamalai University, for their assistance with this research.
References
- Ipshita S, Kurian IG, Dileep P, Kumar S, Singh P, Pradeep AR. One percent alendronate and Aloe vera gel local host modulating agents in chronic periodontitis patients with class II furcation defects: a randomized, controlled clinical trial. J Investig Clin Dent 2018; 9(3):e12334. doi: 10.1111/jicd.12334 [Crossref] [ Google Scholar]
- Bhansali RS. Non-surgical periodontal therapy: an update on current evidence. World J Stomatol 2014; 3(4):38-51. doi: 10.5321/wjs.v3.i4.38 [Crossref] [ Google Scholar]
- Graziani F, Karapetsa D, Alonso B, Herrera D. Nonsurgical and surgical treatment of periodontitis: how many options for one disease?. Periodontol 2000 2017; 75(1):152-88. doi: 10.1111/prd.12201 [Crossref] [ Google Scholar]
- Keestra JA, Grosjean I, Coucke W, Quirynen M, Teughels W. Non-surgical periodontal therapy with systemic antibiotics in patients with untreated chronic periodontitis: a systematic review and meta-analysis. J Periodontal Res 2015; 50(3):294-314. doi: 10.1111/jre.12221 [Crossref] [ Google Scholar]
- Ashouri Moghaddam A, Radafshar G, Jahandideh Y, Kakaei N. Clinical evaluation of effects of local application of Aloe vera gel as an adjunct to scaling and root planning in patients with chronic periodontitis. J Dent (Shiraz) 2017; 18(3):165-72. [ Google Scholar]
- Greenstein G. Nonsurgical periodontal therapy in 2000: a literature review. J Am Dent Assoc 2000; 131(11):1580-92. doi: 10.14219/jada.archive.2000.0087 [Crossref] [ Google Scholar]
- John MT, Michalowicz BS, Kotsakis GA, Chu H. Network meta-analysis of studies included in the clinical practice guideline on the nonsurgical treatment of chronic periodontitis. J Clin Periodontol 2017; 44(6):603-11. doi: 10.1111/jcpe.12726 [Crossref] [ Google Scholar]
- Moro MG, Silveira Souto ML, Franco GC, Holzhausen M, Pannuti CM. Efficacy of local phytotherapy in the nonsurgical treatment of periodontal disease: a systematic review. J Periodontal Res 2018; 53(3):288-97. doi: 10.1111/jre.12525 [Crossref] [ Google Scholar]
- Palombo EA. Traditional medicinal plant extracts and natural products with activity against oral bacteria: potential application in the prevention and treatment of oral diseases. Evid Based Complement Alternat Med 2011; 2011:680354. doi: 10.1093/ecam/nep067 [Crossref] [ Google Scholar]
- Thornhill MH, Dayer MJ, Durkin MJ, Lockhart PB, Baddour LM. Risk of adverse reactions to oral antibiotics prescribed by dentists. J Dent Res 2019; 98(10):1081-7. doi: 10.1177/0022034519863645 [Crossref] [ Google Scholar]
- Zandbergen D, Slot DE, Cobb CM, Van der Weijden FA. The clinical effect of scaling and root planing and the concomitant administration of systemic amoxicillin and metronidazole: a systematic review. J Periodontol 2013; 84(3):332-51. doi: 10.1902/jop.2012.120040 [Crossref] [ Google Scholar]
- Eid Abdelmagyd HA, Ram Shetty DS, Musa Musleh Al-Ahmari DM. Herbal medicine as adjunct in periodontal therapies-a review of clinical trials in past decade. J Oral Biol Craniofac Res 2019; 9(3):212-7. doi: 10.1016/j.jobcr.2019.05.001 [Crossref] [ Google Scholar]
- Bhat G, Kudva P, Dodwad V. Aloe vera: nature’s soothing healer to periodontal disease. J Indian Soc Periodontol 2011; 15(3):205-9. doi: 10.4103/0972-124x.85661 [Crossref] [ Google Scholar]
- Pradeep AR, Garg V, Raju A, Singh P. Adjunctive local delivery of Aloe vera gel in patients with type 2 diabetes and chronic periodontitis: a randomized, controlled clinical trial. J Periodontol 2016; 87(3):268-74. doi: 10.1902/jop.2015.150161 [Crossref] [ Google Scholar]
- Al-Maweri SA, Nassani MZ, Alaizari N, Kalakonda B, Al-Shamiri HM, Alhajj MN. Efficacy of Aloe vera mouthwash versus chlorhexidine on plaque and gingivitis: a systematic review. Int J Dent Hyg 2020; 18(1):44-51. doi: 10.1111/idh.12393 [Crossref] [ Google Scholar]
- Vogler BK, Ernst E. Aloe vera: a systematic review of its clinical effectiveness. Br J Gen Pract 1999; 49(447):823-8. [ Google Scholar]
- Mangaiyarkarasi SP, Manigandan T, Elumalai M, Cholan PK, Kaur RP. Benefits of Aloe vera in dentistry. J Pharm Bioallied Sci 2015; 7(Suppl 1):S255-9. doi: 10.4103/0975-7406.155943 [Crossref] [ Google Scholar]
- Sethi S, Sethi T, Bhusan K, Kabrawala P, Kumar P, Sharma N. Assessment of the efficacy of Aloe vera gel in chronic periodontitis patients: a clinical and microbiological study. J Pharm Biomed Sci 2015; 5(7):598-608. [ Google Scholar]
- Rathod S, Mehta P, Sarda T, Raj A. Clinical efficacy of Aloe vera chip as an adjunct to nonsurgical therapy in the treatment of chronic periodontitis. Int J Res Ayurveda Pharm 2015; 6(4):516-9. doi: 10.7897/2277-4343.06498 [Crossref] [ Google Scholar]
- Singh P, Jain M, Saxena V, Sharva V, Boddun M, Jain N. Evaluation of local–delivery system containing 80% Aloe vera gel used as an adjunct to scaling and root planning in chronic periodontitis: a clinical study. Dent Oral Maxillofac Res 2019; 5(4):1-5. doi: 10.15761/domr.1000309 [Crossref] [ Google Scholar]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. PLoS Med 2021; 18(3):e1003583. doi: 10.1371/journal.pmed.1003583 [Crossref] [ Google Scholar]
- Higgins JP, Thomas J, Chandler J, et al. Cochrane Handbook for Systematic Reviews of Interventions Version 6.2. John Wiley & Sons; 2021.
- Rithesh K, Deepthi R. Comparative evaluation of clinical efficacy of Aloe vera chip as an adjunct to nonsurgical therapy in the treatment of chronic periodontitis. J Nanosci Nanotechnol Res 2021; 5(1):1-7. [ Google Scholar]
- Choudhary A, Chandrashekar KT, Mishra R, Tripathi VD, Hazari V, Trivedi A. Effect of aloin (Aloe vera extract) on the levels of Porphyromonasgingivalis and Aggregatibacteractinomycetemcomitans in chronic generalized periodontitis: a clinical & microbiological study. Int J Adv Res 2019; 7(11):693-701. doi: 10.21474/ijar01/10060 [Crossref] [ Google Scholar]
- Gupta S, Singh P, Janardhana Amaranath BJ, Johnson L, Das N, Tripathi A. Comparison of the efficacy of subgingival irrigation by Aloe vera and 0.2% chlorhexidine (CHX) as an adjunct to nonsurgical therapy in chronic periodontitis subjects. J Cardiovasc Dis Res 2021; 12(6):2357-63. [ Google Scholar]
- Sharma N, Dayakar M, Bhat S, Pai PG. Aloe vera and probiotics in treatment of chronic periodontitis patients: a clinicoradiographic study. RUHS J Health Sci 2018; 3(1):24-9. doi: 10.37821/ruhsjhs.3.1.2018.24-29 [Crossref] [ Google Scholar]
- Sahgal A, Chaturvedi SS, Bagde H, Agrawal P, Suruna R, Limaye M. A randomized control trial to evaluate efficacy of anti-bacterial and anti-inflammatory effect of Aloe vera, pomegranate and chlorhexidine gel against periodontopathogens. J Int Oral Health 2015; 7(11):33-6. [ Google Scholar]
- Penmetsa GS, Subbareddy B, Mopidevi A, Arunbhupathi P, Baipalli V, Pitta S. Comparing the effect of combination of 1% ornidazole and 0.25% chlorhexidine gluconate (OrnigreatTM) gel and Aloe vera gel in the treatment of chronic periodontitis: a randomized, single-blind, split-mouth study. Contemp Clin Dent 2019; 10(2):226-31. doi: 10.4103/ccd.ccd_407_18 [Crossref] [ Google Scholar]
- Kumar A, Sunkara MS, Pantareddy I, Sudhakar S. Comparison of plaque inhibiting efficacies of Aloe vera and propolis tooth gels: a randomized PCR study. J Clin Diagn Res 2015; 9(9):Zc01-3. doi: 10.7860/jcdr/2015/13185.6413 [Crossref] [ Google Scholar]
- Hermanto NR, Syaify A, Sudibyo Sudibyo. Pengaruh Aplikasi Gel Aloe vera Sebagai Bahan Tambahan Scaling Dan Root Planing Terhadap Penyembuhan Jaringan Periodontal Pada Perawatan Periodontitis Kronis (Kajian pada Bleeding on Probing, Pocket Depth, dan Clinical Attachment Level). J Kedokt Gigi 2015; 6(3):307-14. [ Google Scholar]
- Bommireddy VS, Marella Y, Chandu VC, Baddam VR, Bommireddy VS. Aloe vera gel in chronic periodontitis: a clinico-microbiological study. Int Dent J 2023; 73(Suppl 1):S47. doi: 10.1016/j.identj.2023.07.680 [Crossref] [ Google Scholar]
- Sayar F, Farahmand AH, Rezazadeh M. Clinical efficacy of Aloe vera toothpaste on periodontal parameters of patients with gingivitis-a randomized, controlled, single-masked clinical trial. J Contemp Dent Pract 2021; 22(3):242-7. doi: 10.5005/jp-journals-10024-3059 [Crossref] [ Google Scholar]
- Elsadek MF, Ahmed BM, Eskandrani RM, Fahmy TS. Clinical and microbiological outcomes of topical Aloe vera gel vs. photochemotherapy as an adjunct to non-surgical periodontal treatment in periodontitis. Planta Med Int Open 2020; 7(3):e100-5. doi: 10.1055/a-1159-0738 [Crossref] [ Google Scholar]
- Vijay S, Meena R, Chatterjee D, Soangra R, Goyal A, Prakash V. Local drug delivery of Aloe vera gel in chronic periodontitis patient. Univ J Dent Sci 2022; 8(3):3206. doi: 10.21276//ujds.2022.8.3.7 [Crossref] [ Google Scholar]
- Dodwad V, Arora K. Effects of Aloe vera gel, Aloe vera irrigation in treatmentof chronic periodontitis-a clinico-microbiological study. Kerala Dent J 2011; 34(1):48-51. [ Google Scholar]
- Abdelmonem HM, Khashaba OH, Al-Daker MA, Moustafa MD. Effects of Aloe vera gel as an adjunctive therapy in the treatment of chronic periodontitis: a clinical and microbiologic study. Mansoura J Dent 2014; 1(3):11-9. [ Google Scholar]
- Sangwan N, Baiju CS, Bansal S, Gupta G, Mavi S. Comparative evaluation of effect of locally delivered Aloe vera gel with turmeric gel as an adjunct to scaling and root planing in the treatment of chronic periodontitis: a clinical study. IOSR J Dent Med Sci 2017; 16(8):78-83. doi: 10.9790/0853-1608117883 [Crossref] [ Google Scholar]
- Nazir S, Kumar C. The effect of Aloe vera in patient with chronic periodontitis. Pak J Med Dent 2018; 7(4):45-9. [ Google Scholar]
- Phatale SK, Chavda M. Adjunctive local delivery of Aloe vera gel in the treatment of chronic periodontitis: a clinical study with 3-month follow up. Int J Sci Res 2019; 9(1):55-7. [ Google Scholar]
- Timothy CN, Rajasekar AR. Efficacy of Aloe vera gel as an adjunct to scaling and root planing in the management of chronic periodontitis. Plant Cell Biotechnol Mol Biol 2020; 21(27-28):14-20. [ Google Scholar]
- Katariya C, Rajasekar A. Efficacy of locally delivered Aloe vera hydrogel in patients with chronic periodontitis: a prospective clinical study. Cureus 2024; 16(4):e59109. doi: 10.7759/cureus.59109 [Crossref] [ Google Scholar]
- Sterne JA, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019; 366:l4898. doi: 10.1136/bmj.l4898 [Crossref] [ Google Scholar]
- Qamar Z, Almohana SA, Khalid Alanazi A, Khalid Alanazi A, Almohana AA, Zeeshan T. Clinical evaluation of the effects of topical indocyanine-green mediated photosensitiser vs Aloe vera gel as adjunct therapy to scaling and root planing in chronic periodontitis patients. Oral Health Prev Dent 2021; 19:489-94. doi: 10.3290/j.ohpd.b2082037 [Crossref] [ Google Scholar]
- Tayeb FE, El Rashidy ME, Fahmy RA, Abd El Gaffar MS. Adjunctive treatment with locally delivered Aloe vera gel in patients with chronic periodontitis (a randomized, controlled trial). Alex Dent J 2022; 47(3):42-8. doi: 10.21608/adjalexu.2021.55192.1146 [Crossref] [ Google Scholar]
- Borgohain R, Fatima N, Bagde H, Dhanai A, Mukherjee K, Joshi P. Efficacy of cucurmin and Aloe vera extracts gel as local drugs delivery agents. J Pharm Bioallied Sci 2023; 15(Suppl 2):S981-3. doi: 10.4103/jpbs.jpbs_259_23 [Crossref] [ Google Scholar]
- Faramarzi M, Khorramdel A, Babaloo AR, Sadighi M, Sadaghian A. Effect of topical Aloe vera gel on gingival crevicular fluid interleukin-1 beta and interleukin-17 levels in patients with chronic periodontitis; a double-blind split-mouth randomized clinical trial. Immunopathol Persa 2024; 10(2):e34426. doi: 10.34172/ipp.2023.34426 [Crossref] [ Google Scholar]
- Marella Y, Dhulipalla R, Chandu VC, Adurty C, Kolaparthy L, Nagamani P. Evaluation of Aloe vera gel as a local drug delivery agent in the treatment of chronic periodontitis: a clinical and microbiological study. Ayu 2024; 45(1):26-31. doi: 10.4103/ayu.AYU_246_19 [Crossref] [ Google Scholar]
- Virdi H, Jain S, Sharma S. Effect of locally delivered Aloe vera gel as an adjunct to scaling and root planing in the treatment of chronic periodontitis: a clinical study. Indian J Oral Sci 2012; 3(2):84. doi: 10.4103/0976-6944.106460 [Crossref] [ Google Scholar]
- Singh HP, Sathish G, Babu KN, Vinod KS, Rao HP. Comparative study to evaluate the effectiveness of Aloe vera and metronidazole in adjunct to scaling and root planing in periodontitis patients. J Int Oral Heal 2016; 8(3):374-7. [ Google Scholar]
- Dilliwal H, Agrawal R, Khashu H, Chouksey A. Efficacy of Aloe vera gel delivered locally as an adjunct to scaling and root planing in the treatment of chronic periodontitis: a pilot study. Int J Oral Care Res 2017; 5(3 Suppl):370-7. doi: 10.5005/jp-journals-10051-0136 [Crossref] [ Google Scholar]
- Deepu S, Kumar K, Nayar BR. Efficacy of Aloe vera gel as an adjunct to scaling and root planing in management of chronic localized moderate periodontitis: a randomized clinical trial. Int J Oral Care Res 2018; 6(2):49-53. [ Google Scholar]
- Kurian IG, Dileep P, Ipshita S, Pradeep AR. Comparative evaluation of subgingivally-delivered 1% metformin and Aloe vera gel in the treatment of intrabony defects in chronic periodontitis patients: a randomized, controlled clinical trial. J Investig Clin Dent 2018; 9(3):e12324. doi: 10.1111/jicd.12324 [Crossref] [ Google Scholar]
- Agrawal C, Parikh H, Virda R, Duseja S, Shah M, Shah K. Effects of Aloe vera gel as an adjunctive therapy in the treatment of chronic periodontitis–a randomized clinical trial. World J Adv Sci Res 2019; 2(1):154-68. [ Google Scholar]
- McGuinness LA, Higgins JP. Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods 2021; 12(1):55-61. doi: 10.1002/jrsm.1411 [Crossref] [ Google Scholar]
- Surjushe A, Vasani R, Saple DG. Aloe vera: a short review. Indian J Dermatol 2008; 53(4):163-6. doi: 10.4103/0019-5154.44785 [Crossref] [ Google Scholar]
- Ahmadi A. Potential prevention: Aloe vera mouthwash may reduce radiation-induced oral mucositis in head and neck cancer patients. Chin J Integr Med 2012; 18(8):635-40. doi: 10.1007/s11655-012-1183-y [Crossref] [ Google Scholar]
- Dhingra K. Aloe vera herbal dentifrices for plaque and gingivitis control: a systematic review. Oral Dis 2014; 20(3):254-67. doi: 10.1111/odi.12113 [Crossref] [ Google Scholar]
- Jadhav AN, Rathod SR, Kolte AP, Bawankar PV. Effect of Aloe vera as a local drug delivery agent in the management of periodontal diseases: a systematic review and meta-analysis. J Indian Soc Periodontol 2021; 25(5):372-8. doi: 10.4103/jisp.jisp_40_21 [Crossref] [ Google Scholar]
- Gupta RK, Gupta D, Bhaskar DJ, Yadav A, Obaid K, Mishra S. Preliminary antiplaque efficacy of Aloe vera mouthwash on 4-day plaque re-growth model: randomized control trial. Ethiop J Health Sci 2014; 24(2):139-44. doi: 10.4314/ejhs.v24i2.6 [Crossref] [ Google Scholar]
- Ndhlala AR, Amoo SO, Stafford GI, Finnie JF, Van Staden J. Antimicrobial, anti-inflammatory and mutagenic investigation of the South African tree aloe (Aloe barberae). J Ethnopharmacol 2009; 124(3):404-8. doi: 10.1016/j.jep.2009.05.037 [Crossref] [ Google Scholar]
- Barrantes E, Guinea M. Inhibition of collagenase and metalloproteinases by aloins and aloe gel. Life Sci 2003; 72(7):843-50. doi: 10.1016/s0024-3205(02)02308-1 [Crossref] [ Google Scholar]
- Kudalkar MD, Nayak A, Bhat KS, Nayak RN. Effect of Azadirachtaindica (Neem) and Aloe vera as compared to subantimicrobial dose doxycycline on matrix metalloproteinases (MMP)-2 and MMP-9: An in-vitro study. Ayu 2014; 35(1):85-9. doi: 10.4103/0974-8520.141947 [Crossref] [ Google Scholar]