J Adv Periodontol Implant Dent. 16(2):139-143.
doi: 10.34172/japid.2024.014
Research Article
Quantitative evaluation of the canalis sinuosus relative to adjacent structures in cone-beam computed tomography images
Sahar Jabali Investigation, Methodology, Supervision, Validation, Writing – review & editing, 1 
Sajjad Pishva Data curation, Visualization, Writing – original draft, Writing – review & editing, 1
Roghieh Bardal Data curation, Formal analysis, Software, Visualization, Writing – original draft, Writing – review & editing, 2
Farough Bahrami Investigation, Resources, Validation, Writing – review & editing, 3
Maryam Mostafavi Conceptualization, Investigation, Methodology, Project administration, Resources, Writing – review & editing, 4, * 
Author information:
1Department of Periodontology, School of Dentistry, Urmia University of Medical Sciences, Urmia, Iran
2Department of Oral and Maxillofacial Radiology, Dental Caries Prevention Research Center, Qazvin University of Medical Sciences, Qazvin, Iran
3Department of Endodontics, School of Dentistry, Isfahan University of Medical Sciences, Isfahan, Iran
4Department of Oral and Maxillofacial Radiology, School of Dentistry, Urmia University of Medical Sciences, Urmia, Iran
Abstract
Background.
Careful anatomical investigation of canalis sinuosus (CS) is essential to prevent damage to blood vessels and nerves in this area during surgical procedures, such as placing dental implants in the anterior maxillary region. This study investigated the relationship and distance between the CS and its adjacent structures.
Methods.
A total of 400 cone-beam computed tomography (CBCT) images of Iranian adults aged 20–86 years were included in this retrospective study. Two observers assessed all the images twice with a time interval of one month. The closest tooth to the CS, its position relative to the CS, and distance measurements of the CS from adjacent structures were determined.
Results.
CS was found in 10.5% of all images. The mean diameter of the canal was 1.06±0.29 mm, which was not significantly different between the age groups, right and left sides, or genders. The most common location of CS was mid-position relative to the upper lateral incisors. In linear measurements, only the distance from the CS to the buccal cortical plate and perpendicular to the nasopalatine canal exhibited a significant difference between the two sexes, with no significant difference between the right and left sides.
Conclusion.
CS location was significantly more palato-lateral in males. There was no significant difference in the prevalence between the two sexes.
Keywords: Anatomic variations, Cone-beam computed tomography, Maxillary nerve
Copyright and License Information
© 2024 The Author(s).
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Funding Statement
There was no financial support for the study.
Introduction
The anterior region of the maxilla undergoes many surgical interventions. Dental implant placement, surgeries of supernumerary impacted teeth and cysts, and orthognathic surgeries are some of these interventions in the anterior maxilla.1 However, the most important of all these is the increasing demand for dental implants. Thus, a more precise anatomical investigation of this segment is essential due to the presence of canalis sinuosus (CS) in the anterior maxilla.2 CS is a neurovascular canal about 2 mm in diameter, which carries a branch of nerves of the infraorbital canal, the anterior superior alveolar nerve (ASA), and related vessels.3,4 The infraorbital nerve is a branch of the maxillary nerve, which is the second branch of the fifth cranial nerve, i.e., the trigeminal nerve. The skin distribution of the infraorbital nerve extends to the upper lip, cheeks, lower eyelids, outer nose, and nasal cavity.5
On cone-beam computed tomography (CBCT) images, CS is a curved bone canal originating laterally from the infraorbital canal. It passes through an internal and anterior course to reach the maxillary anterior region, passes through the lateral wall of the nose, and is placed in the marginal part of the nasal cavity floor; then, lateral canals branch off, eventually opening next to the incisor canal in the palate.6 CS detection is important because damage to such structures might cause sensory disorders. In addition, such structures may be mistaken for other anatomical structures or lesions, leading to unnecessary or incorrect procedures.7 Therefore, accurately identifying the anatomy of the face, mouth, and jaws and using radiographic images, specifically CBCT in surgical procedures, are necessary to avoid the destruction of blood vessels and nerves in this area.8
The anatomy of the CS9-13 and its accessory canals14-19 has been evaluated in numerous studies. A systematic review study conducted in 2023 considered CS and its accessory canals as anatomic structures due to their high prevalence.20 However, a few studies have quantitatively evaluated the canal’s relationship with adjacent structures.4 Therefore, this study investigated the exact position of CS relative to adjacent teeth and its distance from adjacent anatomical structures in CBCT images of an Iranian population.
Methods
The present retrospective study was conducted on 400 CBCT images of the anterior maxilla of Iranian patients referred to a private dental and maxillofacial radiology center in Urmia, Iran.
The inclusion criteria: (1) a chronological age of 12−90, (2) no history of systemic disease due to osteoporosis, (3) and good diagnostic quality of images.
The exclusion criteria: the images of edentulous patients and patients with dentoalveolar fractures, pathologic conditions, dental implants, or bone grafting in the anterior maxilla.
The CBCT images were captured using an 8-cm field of view of Planmeca Promax 3D mid (Helsinki, Finland) with the following conditions: voxel size: 200 μm; time: 12 s; mA: 10; kVp: 90.
Two observers investigated all the images twice with a time interval of one month. The first observer was an experienced periodontist, and the second observer was an experienced oral and maxillofacial radiologist. Observations and measurements were carried out by Planmeca Romexis software version 3.8.1. The presence of CS was defined in axial and sagittal planes, and its clear extension was confirmed in the coronal sections. CS diameter was measured on the axial plane. Canals with a diameter of > 1 mm and a definite extension to the infraorbital canal were considered (Figure 1). Slice thickness and interval were 0.5 in all the sections. The axial plane in which the CS had the largest diameter was chosen to measure the distance of the CS to the adjacent teeth and the nasopalatine canal. The tooth with the closest distance to the CS was considered the main tooth; then, the mesial, mid, or distal position of the main tooth related to the CS was determined. The distances of CS from the nasal floor, ridge crest, buccal cortical plate, and the distance of canal extension from the main tooth apex were measured on the cross-sections perpendicular to the axial plane at the CS site (Figures 2 and 3).
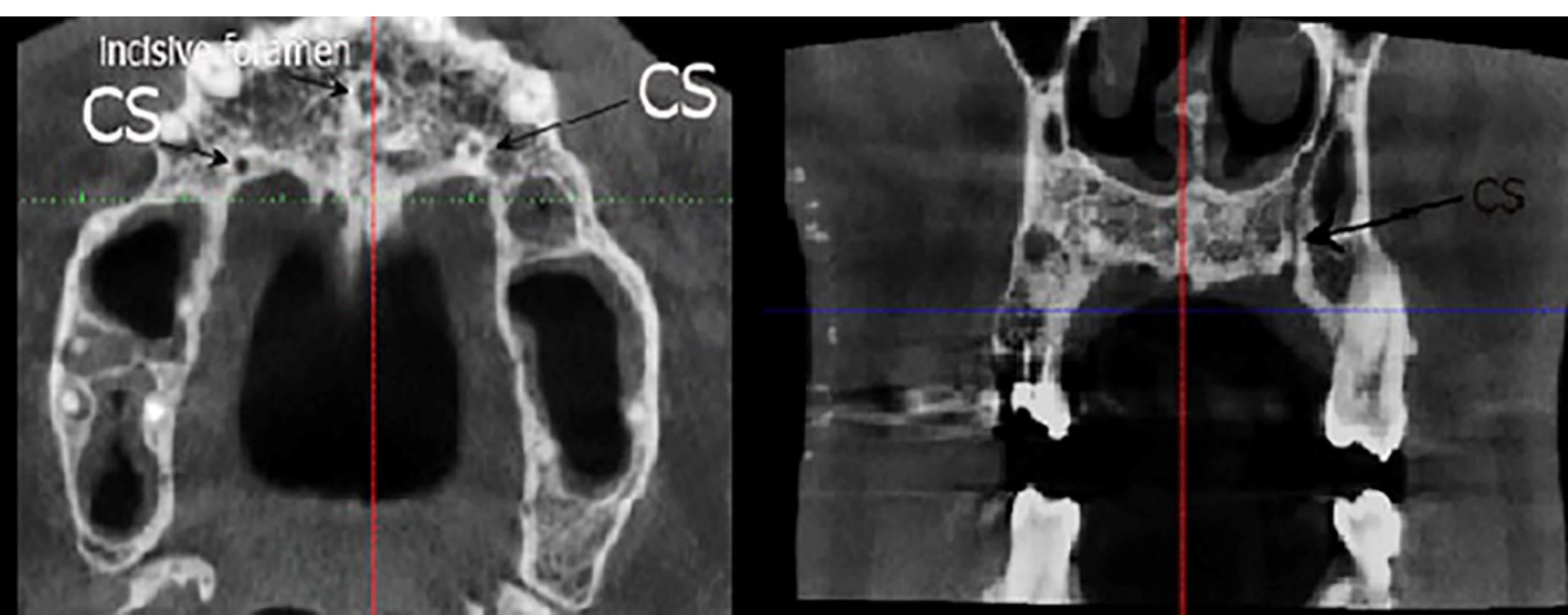
Figure 1.
Axial and coronal views of the CS
.
Axial and coronal views of the CS
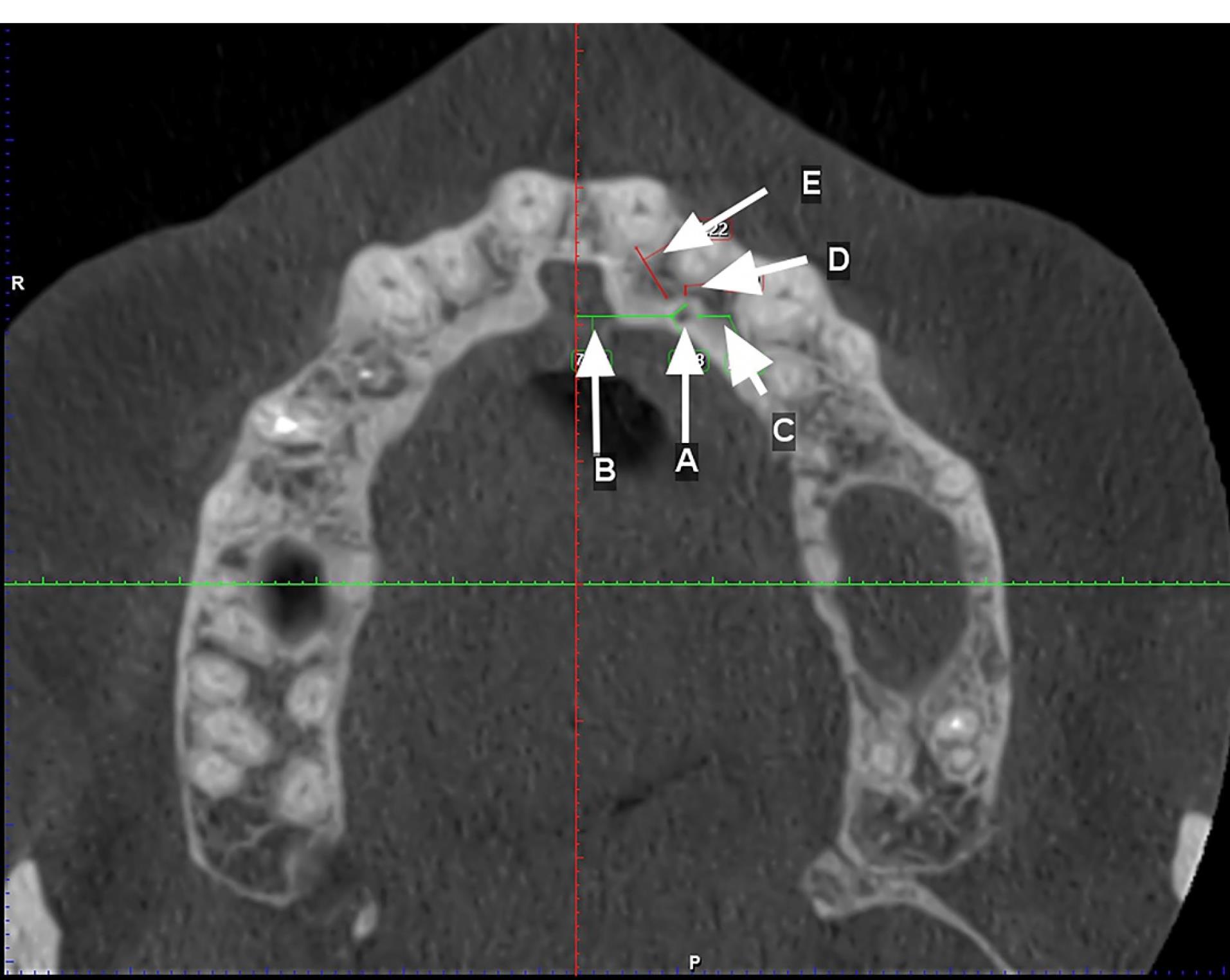
Figure 2.
Linear measurements made in the axial plane: A, the CS diameter; B, the CS distance from the perpendicular to the nasopalatine canal; C, the CS distance from the distal tooth; D, the CS distance from the main tooth; E, the CS distance from the mesial toot
.
Linear measurements made in the axial plane: A, the CS diameter; B, the CS distance from the perpendicular to the nasopalatine canal; C, the CS distance from the distal tooth; D, the CS distance from the main tooth; E, the CS distance from the mesial toot
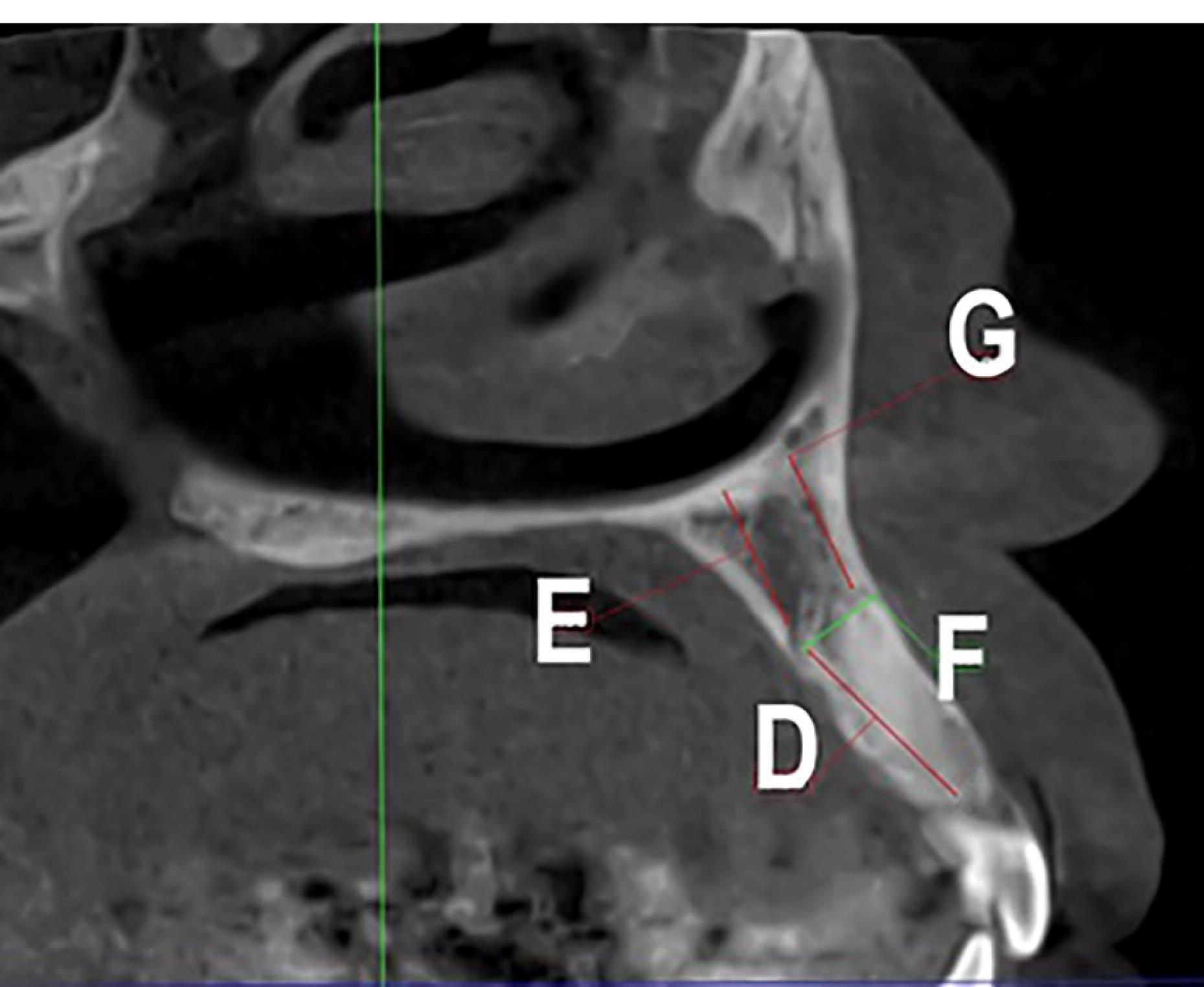
Figure 3.
Linear measurements made in the cross-section: D, the CS distance from the crest ridge; E, the CS distance from the nasal cavity floor; F, the CS distance from the buccal cortical plate; G, the distance of canal extension from the main tooth apex
.
Linear measurements made in the cross-section: D, the CS distance from the crest ridge; E, the CS distance from the nasal cavity floor; F, the CS distance from the buccal cortical plate; G, the distance of canal extension from the main tooth apex
Intra- and inter-observer reliability was evaluated in 10% of the CBCT images after two weeks using the intraclass correlation coefficient (ICC).
Statistical analysis
The data were analyzed with SPSS 22 using descriptive statistics, i.e., maximum, minimum, mean, and standard deviation. The ICC value was ˃0.80 for both intra- and inter-observer reliabilities. Pearson’s correlation coefficient was used to determine the relation between two quantitative variables. Fisher’s exact test was used to compare CS distribution in terms of sex and location. T-test was used to compare distance measurements between males and females or between the right and left sides. P ≥ 0.05 was considered statistically insignificant.
Results
CBCT images of 400 patients were investigated, with 185 males (46.3%) and 215 (53.7%) females. The mean age of the patients was 43.06 ± 13.60, with a range of 20–86 years. Forty-two patients (10.5%) had at least one CS with a clear extension towards the infraorbital canal, with a diameter of > 1 mm; 20 (47.6%) were female, and 22 (53.4%) were male. In 13 patients (30.95%), the canal was bilateral, and in 29 (69.05%), the canal was unilateral. In 25 (86.2%) patients, the canal was on the right side, and in 4 (13.80%), the canal was on the left side; generally, 55 canals were observed in images.
Table 1 shows the mean diameters of CS in both sexes. There was no significant difference in the frequency of cases between the two genders (P > 0.05). No significant correlation was observed between CS diameter and age (P = 0.101) or sex (P = 0.284). CS was more frequent on the right side than on the left side, but this difference was not significant (P > 0.05) (Table 2). The CS had the closest distance to the lateral incisor in most cases. The mid-position of the CS compared to the main tooth was significantly more common than other positions (P = 0.04).
Table 1.
CS diameter in mm according to sex
|
Sex
|
Number
|
Mean (SD)
|
Minimum
|
Maximum
|
| Male |
28 |
1.10 (0.31) |
0.67 |
1.75 |
| Female |
27 |
1.02 (0.28) |
0.75 |
1.81 |
| Total |
55 |
1.06 (0.29) |
0.60 |
1.81 |
Table 2.
Frequencies (%) of CS in the patients according to sex, side, and position
|
|
Sex
|
Side
|
Position
|
|
Male (%)
|
Female (%)
|
Right (%)
|
Left (%)
|
Mesial-position (%)
|
Mid-position (%)
|
Distal-position (%)
|
| Central Incisor |
1 (1.8) |
2 (3.6) |
2 (3.6) |
1 (1.8) |
0 (0.0) |
1 (1.8) |
2 (3.6) |
| Lateral Incisor |
12 (21.8) |
17 (30.9) |
18 (32.7) |
11 (20) |
4 (7.3) |
20 (36.3) |
5 (9.1) |
| Canine |
11 (20) |
7 (12.7) |
13 (23.6) |
5 (9.1) |
1 (1.8) |
8 (14.6) |
9 (16.5) |
| First Premolar |
4 (7.3) |
1 (1.8) |
5 (9.1) |
0 (0.0) |
2 (3.6) |
1 (1.8) |
2 (3.6) |
| Total |
28 (50.9) |
27 (49.1) |
38 (69.1) |
17 (30.9) |
7 (12.7) |
30 (54.5) |
18 (32.8) |
|
P value |
0.32 |
0.41 |
0.04 |
The average distances of CS from the nasal floor, ridge crest, buccal cortical plate, main tooth apex, and nasopalatine canal were higher in males than in females; this difference was not statistically significant except for the buccal cortical plate distance and perpendicular distance to the nasopalatine canal (Table 3). The distance of CS from neighboring structures on the right and left sides was not statistically significant (P > 0.05).
Table 3.
Means and standard deviations (SDs) of the distances between CS and anatomic landmarks according to sex and side
|
Anatomic landmark
|
Sex
|
P
value
|
Side
|
P
value
|
Total
|
|
Male
|
Female
|
Right
|
Left
|
| Nasal cavity |
11.58 (3.63) |
10.17(3.61) |
0.15 |
11.24 (3.48) |
10.66(3.80) |
0.58 |
10.89 (3.66) |
| Buccal cortical |
8.92 (1.58) |
8.10 (0.98) |
0.02 |
8.46 (1.29) |
8.56 (1.44) |
0.80 |
8.52 (1.37) |
| Ridge crest |
10.48 (4.13) |
9.30 (2.81) |
0.22 |
9.34 (3.10) |
10.27 (3.84) |
0.34 |
9.90 (3.56) |
| Main tooth apex |
4.60 (2.31) |
4.21 (1.28) |
0.44 |
4.58 (1.51) |
4.30 (2.09) |
0.57 |
4.41 (1.87) |
| Main tooth |
2.19 (1.88) |
1.66 (0.67) |
0.16 |
1.83 (1.20) |
2.00 (1.58) |
0.66 |
1.93 (1.43) |
| Distal tooth |
5.28 (1.30) |
4.72 (1.70) |
0.17 |
5.32 (1.58) |
4.80 (1.49) |
0.25 |
4.99 (1.53) |
| Mesial tooth |
4.96 (1.70) |
4.52 (1.23) |
0.27 |
4.68 (1.16) |
4.77 (1.67) |
0.81 |
4.73 (1.48) |
| Perpendicular to the nasopalatine canal |
9.48 (3.19) |
7.26 (2.20) |
0.00 |
9.14 (3.40) |
7.90 (2.54) |
0.18 |
8.39 (2.95) |
Discussion
CS is a branch of the infraorbital nerve, which is the maxillary division of the trigeminal nerve. Damage to this canal during surgery can lead to complications such as bleeding and paresthesia. CS can be detected in special imaging modalities such as thin sections of CBCT.4
This study evaluated the location and distance of CS relative to adjacent structures in the Iranian population because of anatomical variations between different populations.
The prevalence of CS in this study was 10%, which was close to a study by de Oliveira-Santos et al. (15.7%)21; this prevalence was about 35% in a study by Manhães Júnior et al,4 66.5% in a study by Aoki et al,13 88% in a study by Wanzeler et al,5 and 98.5% in a study by Yeap et al.22 However, the prevalence of CS in a study by Gurler et al23 was 100%. The possible reasons for this discrepancy include differences in the slice thickness of the CBCT images,23 the software used, sample size, and the content of studies.11 In addition, in this study, cases traceable to the infraorbital canal with a diameter of > 1 mm were selected, which could be another reason for the difference.
The canal was bilateral in 13 patients (30.95%) of the 42 patients with CS. The frequency percentage of bilateral cases of CS was various in other literature as follows: de Oliveira-Santos et al.21 reported 21.4%, Manhães et al4 reported 24.3%, Aoki et al13 reported 54.1%, and Gurler et al23 reported 100%.
There was no significant difference in the overall frequency of CS on both sides (P = 0.41), consistent with the Manhães et al. study.
Gender distribution of CS was not statistically significant, consistent with studies by Gurler et al,23 Von Arks et al,6 Machado et al,19 and Wanzeler et al.5 In a study by Anatoly et al,24 the prevalence of CS was significantly higher in females, while this prevalence was significantly higher in males in Aoki et al. study.13
The mean (SD) diameter of CS was 1.06 (0.26) mm, which was significantly (P = 0.284) higher in males [mean (SD) diameter in males = 1.10 (0.31) vs. females = 1.02 (0.28)]. In the study by Aoki et al,13 this difference was not significant, either. Gurler et al.23 reported a significantly higher mean diameter of CS in males (P = 0.001).
Because of the difficulty of some cases in precisely attributing the CS to the specific tooth,16 Beyzade et al25 modified the classification used by Oliveira-Santos et al.21 For the same reason, in this study, CS’s distance to the neighboring teeth was determined in axial plane in which the CS had the most diameter, at first. The position of the CS with regard to the closest tooth was determined at the second. CS was most related to the mid-position of lateral incisors. CS was more commonly associated with this tooth in other populations.4,11,22,24
In this study, CS-to-the-buccal cortical plate and CS-perpendicular-to-nasopalatine canal distances were significantly higher in males, so the CS location was more palato-lateral. In the Manhães Júnior et al4 study, the nasal cavity distance was higher than in our study, and the ridge crest and the buccal cortical plate distances were lower than in our study, so the CS was located in a more buccal position and closer to the crest in Manhães Júnior and colleagues’ study.
Conclusion
The prevalence, diameter, and most of the linear distances of the CS to the adjacent structures were not significantly different between the two genders. However, CS had a significantly more palato-lateral position in males. There were variations in the prevalence, location, and linear distances between different populations.
Acknowledgments
The authors would like to thank Dr. Majid Abdolrahimi for his cooperation in writing the manuscript.
Competing Interests
The authors declare that they have no competing interests.
Consent for Publication
Not applicable.
Data Availability Statement
The data that support our results are available upon reasonable request from the corresponding author, Maryam Mostafavi.
Ethical Approval
This study was approved by the Ethics Committee of Urmia University of Medical Sciences with the ethical number of IR.UMSU.REC.1397.064. There was no conflict with ethical considerations.
References
- Suter VG, Sendi P, Reichart PA, Bornstein MM. The nasopalatine duct cyst: an analysis of the relation between clinical symptoms, cyst dimensions, and involvement of neighboring anatomical structures using cone beam computed tomography. J Oral Maxillofac Surg 2011; 69(10):2595-603. doi: 10.1016/j.joms.2010.11.032 [Crossref] [ Google Scholar]
- Kim S, Kratchman S. Modern endodontic surgery concepts and practice: a review. J Endod 2006; 32(7):601-23. doi: 10.1016/j.joen.2005.12.010 [Crossref] [ Google Scholar]
- Jones FW. The anterior superior alveolar nerve and vessels. J Anat 1939; 73(Pt 4):583-91. [ Google Scholar]
- Manhães Júnior LR, Villaça-Carvalho MF, Moraes ME, de Castro Lopes SL, Silva MB, Junqueira JL. Location and classification of canalis sinuosus for cone beam computed tomography: avoiding misdiagnosis. Braz Oral Res 2016; 30(1):e49. doi: 10.1590/1807-3107BOR-2016.vol30.0049 [Crossref] [ Google Scholar]
- Wanzeler AM, Marinho CG, Alves Junior SM, Manzi FR, Tuji FM. Anatomical study of the canalis sinuosus in 100 cone beam computed tomography examinations. Oral Maxillofac Surg 2015; 19(1):49-53. doi: 10.1007/s10006-014-0450-9 [Crossref] [ Google Scholar]
- von Arx T, Lozanoff S. Anterior superior alveolar nerve (ASAN). Swiss Dent J 2015; 125(11):1202-9. doi: 10.61872/sdj-2015-11-01 [Crossref] [ Google Scholar]
- Vâlcu M, Rusu MC, Sendroiu VM, Didilescu AC. The lateral incisive canals of the adult hard palate - aberrant anatomy of a minor form of clefting?. Rom J Morphol Embryol 2011; 52(3):947-9. [ Google Scholar]
- Chrcanovic BR, Abreu MH, Custódio AL. A morphometric analysis of supraorbital and infraorbital foramina relative to surgical landmarks. Surg Radiol Anat 2011; 33(4):329-35. doi: 10.1007/s00276-010-0698-1 [Crossref] [ Google Scholar]
- Neves FS, Crusoé-Souza M, Franco LC, Caria PH, Bonfim-Almeida P, Crusoé-Rebello I. Canalis sinuosus: a rare anatomical variation. Surg Radiol Anat 2012; 34(6):563-6. doi: 10.1007/s00276-011-0907-6 [Crossref] [ Google Scholar]
- Arruda JA, Silva P, Silva L, Álvares P, Silva L, Zavanelli R. Dental implant in the canalis sinuosus: a case report and review of the literature. Case Rep Dent 2017; 2017:4810123. doi: 10.1155/2017/4810123 [Crossref] [ Google Scholar]
- Ferlin R, Pagin BSC, Yaedú RY. Canalis sinuosus: a systematic review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol 2019; 127(6):545-51. doi: 10.1016/j.oooo.2018.12.017 [Crossref] [ Google Scholar]
- Torres MG, de Faro Valverde L, Vidal MT, Crusoé-Rebello IM. Branch of the canalis sinuosus: a rare anatomical variation--a case report. Surg Radiol Anat 2015; 37(7):879-81. doi: 10.1007/s00276-015-1432-9 [Crossref] [ Google Scholar]
- Aoki R, Massuda M, Zenni LT, Fernandes KS. Canalis sinuosus: anatomical variation or structure?. Surg Radiol Anat 2020; 42(1):69-74. doi: 10.1007/s00276-019-02352-2 [Crossref] [ Google Scholar]
- Orhan K, Gorurgoz C, Akyol M, Ozarslanturk S, Avsever H. An anatomical variant: evaluation of accessory canals of the canalis sinuosus using cone beam computed tomography. Folia Morphol (Warsz) 2018; 77(3):551-7. doi: 10.5603/FM.a2018.0003 [Crossref] [ Google Scholar]
- Tomrukçu DN, Köse TE. Assesment of accessory branches of canalis sinuosus on CBCT images. Med Oral Patol Oral Cir Bucal 2020; 25(1):e124-30. doi: 10.4317/medoral.23235 [Crossref] [ Google Scholar]
- Ghandourah AO, Rashad A, Heiland M, Hamzi BM, Friedrich RE. Cone-beam tomographic analysis of canalis sinuosus accessory intraosseous canals in the maxilla. Ger Med Sci 2017; 15:Doc20. doi: 10.3205/000261 [Crossref] [ Google Scholar]
- Shah PN, Arora AV, Kapoor SV. Accessory branch of canalis sinuosus mimicking external root resorption: a diagnostic dilemma. J Conserv Dent 2017; 20(6):479-81. doi: 10.4103/jcd.jcd_375_16 [Crossref] [ Google Scholar]
- Shan T, Qu Y, Huang X, Gu L. Cone beam computed tomography analysis of accessory canals of the canalis sinuosus: a prevalent but often overlooked anatomical variation in the anterior maxilla. J Prosthet Dent 2021; 126(4):560-8. doi: 10.1016/j.prosdent.2020.05.028 [Crossref] [ Google Scholar]
- Machado VC, Chrcanovic BR, Felippe MB, Manhães Júnior LR, de Carvalho PS. Assessment of accessory canals of the canalis sinuosus: a study of 1000 cone beam computed tomography examinations. Int J Oral Maxillofac Surg 2016; 45(12):1586-91. doi: 10.1016/j.ijom.2016.09.007 [Crossref] [ Google Scholar]
- de Oliveira-Neto OB, Barbosa FT, de Lima FJ, de Sousa-Rodrigues CF. Prevalence of canalis sinuosus and accessory canals of canalis sinuosus on cone beam computed tomography: a systematic review and meta-analysis. Int J Oral Maxillofac Surg 2023; 52(1):118-31. doi: 10.1016/j.ijom.2022.06.011 [Crossref] [ Google Scholar]
- de Oliveira-Santos C, Rubira-Bullen IR, Monteiro SA, León JE, Jacobs R. Neurovascular anatomical variations in the anterior palate observed on CBCT images. Clin Oral Implants Res 2013; 24(9):1044-8. doi: 10.1111/j.1600-0501.2012.02497.x [Crossref] [ Google Scholar]
- Yeap CW, Danh D, Chan J, Parashos P. Examination of canalis sinuosus using cone beam computed tomography in an Australian population. Aust Dent J 2022; 67(3):249-61. doi: 10.1111/adj.12910 [Crossref] [ Google Scholar]
- Gurler G, Delilbasi C, Ogut EE, Aydin K, Sakul U. Evaluation of the morphology of the canalis sinuosus using cone-beam computed tomography in patients with maxillary impacted canines. Imaging Sci Dent 2017; 47(2):69-74. doi: 10.5624/isd.2017.47.2.69 [Crossref] [ Google Scholar]
- Anatoly A, Sedov Y, Gvozdikova E, Mordanov O, Kruchinina L, Avanesov K. Radiological and morphometric features of canalis sinuosus in Russian population: Cone-Beam Computed Tomography Study. Int J Dent 2019; 2019:2453469. doi: 10.1155/2019/2453469 [Crossref] [ Google Scholar]
- Beyzade Z, Yılmaz HG, Ünsal G, Çaygür-Yoran A. Prevalence, radiographic features and clinical relevancy of accessory canals of the canalis sinuosus in cypriot population: a retrospective Cone-Beam Computed Tomography (CBCT) Study. Medicina (Kaunas) 2022; 58(7):930. doi: 10.3390/medicina58070930 [Crossref] [ Google Scholar]